Conference Venue: Weston A. Price Foundation’s Wise Traditions – 2017 Conference
Hyatt Regency Minneapolis, Minneapolis, Minnesota
Date of Presentation: November 12, 2017
Dr. Knobbe’s Presentation Transcript and Slides
“Today you’re going to hear a revolutionary hypothesis for the cause of macular degeneration.
This is a hypothesis which holds that age-related macular degeneration is not only entirely preventable, but that it may be treatable and even possibly reversible in the early stages, with an ancestral diet.
So what I’m going to show you today is that macular degeneration was once a very rare disorder — and today, it is an epidemic in developed nations, worldwide. And the only thing that’s changed that can account for that, is our diet. That’s the only thing.
So, with that said, I represent Cure AMD Foundation. We are a non-profit organization and our goal is to prevent vision loss, save vision, treat vision through ancestral dietary strategy – through the hypothesis and the research that I’ll present to you today.
My name is Chris Knobbe and I want you to notice, if you would that I’m an MD —
Because when it comes to nutrition, that “MD” means — “Masterfully Dumb” (Crowd Laughter).
You all agree with that?
(Crowd… “Yes!”)
Thank you! We’re on the same page!
Now, in our defense, you know, in four years of medical school, I didn’t get any nutrition education. Well, I take that back. Because one day I fell asleep in 2nd year medical school, for about three minutes, and I looked up to my buddy next to me and I said, ‘What did I miss?’
And he said, ‘You missed the entire nutrition tract.’ (Crowd laughter)
And I said, ‘Are they going to repeat it?’
And he said, ‘No, that’s it.’
So, that’s what we got.
So… the last seven years, I’ve taken it upon myself to try to learn about nutrition. So, hopefully, what I can bring to you today will make a difference – and add to this body of knowledge that this great Weston A. Price Foundation and all of these members can take home.
So, alright… I know you’re not ophthalmologists or optometrists. Let’s start with just the fundamentals.
Age-related macular degeneration, or AMD, is the leading cause of irreversible vision loss and blindness, in developed nations, in people over the age of 65.
This disease, can cause the vision to go from like that on the left, to that on the right.

So these huge central blind spots develop and about 15 to 20 percent of eyes will end up like this.
Today, 20,000 people will develop AMD. And again tomorrow. And the day after that — worldwide. Twenty-thousand per day will come down with a diagnosis of this disease.
So – since 1992, nearly one of every three adults over the age of 75 is currently affected with AMD and globally, one of every eleven adults over the age of 50 now has some degree of AMD. That’s staggering!
So in the United States, by 1994 it was estimated that 15 million Americans were affected with macular degeneration.
It is anticipated that by 2020, 196 million people will be affected worldwide. So we’re really close to that number. More than two million people blind, worldwide, as of 2002 according to the World Health Organization (WHO). So I would estimate that number is closer to three million people, today.
But what do you suppose the lifetime risk of developing AMD was back in the year 1900? Anybody?
(Crowd – inaudible)
Yeah, people are saying two percent – you know – the answer is — almost zero!
One in many thousands [affected by AMD]. Now I’m going to come back and review some of this for you — and I hope I can convince you that this was an incredibly rare disorder.
And the question is, ‘Why?’
How did we go from one in many thousands affected in 1900 — to nearly one in three by 1990?
That’s what I want you to think about as we go through this today.
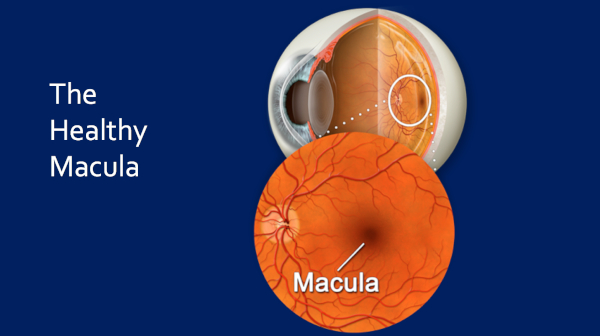
So this is the healthy macula.
Uhmm, so here’s the — retina back here — and this is the macula. This distance is only about 6 millimeters. This is only about one-quarter of an inch, and this accounts for the central ten degrees of your vision. And this is what it looks like when it’s healthy — it looks like that.
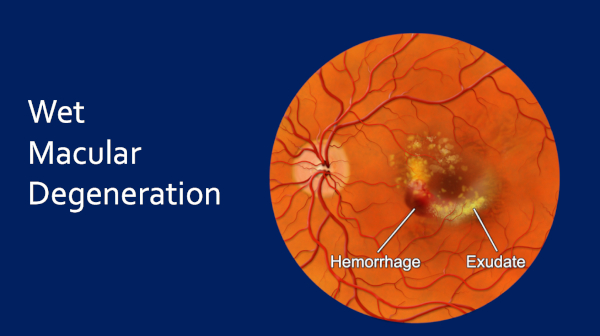
And this is dry macular degeneration.
This is — the enormous majority of the time you’re going to go through the Dry AMD stage first. We see these drusen – these metabolic deposits – and what we call pigmentary disturbance and then this progresses — may progress — onto Wet Macular Degeneration.
This will hit around 15 percent of patients and in the untreated state, this stage of the disease will end up with absolute devastation to the vision. You will have a central blind spot.
And of course, again, the vision can go from like that on the left to this huge central blind area on the right.
The question is — today — is this difference due to diet — and diet alone.
And I will submit to you that everything I have discovered in the last several years suggests that it is entirely diet.
And I will show you why, today.
So, now I know you all know about ancestral diets here [at the Wise Traditions Conference venue], but let me just give you a little bit of my viewpoint. Because, I spent a lot of time trying to understand the history of diets, and to me, an ancestral diet is any diet that existed anywhere on the planet, before 1880.
Why then? Because, before 1880 we had no man-made, processed foods, essentially.
If you went to the grocery story in 1879, what you came home with was meat, fowl, fish, fruit, vegetables, grains, nuts, seeds, dairy — you know — so butter, eggs, and raw milk. Right?
And these foods were grown the way they should be grown. Animals on pasture and foraging, and fruits, vegetables, and grains all grown without herbicides and pesticides, right?
Everything was organic, as well.
Now, contrast that to our Westernized diet.
Now, we all know what it looks like. But the thing is — there is 600,000 food items available in the U.S. today.
So let’s break this down. Because it’s very simple.
About 63 percent of what’s on this American plate today consists of four refined, processed, nutrient-deficient foods, that didn’t exist before 1880, with the exception of sugar in small quantities.
So those four foods though:
Sugar, refined white flour, polyunsaturated vegetable oils, and trans fats.
Those four things became Big Food — and changed the world, forever.
And this, of course, is the reason for all of this chronic, metabolic disease. I know you guys know this.
Uhm, and this is what I’m going to tell you today is the same cause of macular degeneration.
So for decades, what we have seen, in textbooks of ophthalmology, journals, papers — is some version of this statement —
The etiology of AMD is unknown. We don’t know what causes it.
So if we don’t know what causes it, we certainly can’t prevent it, right?
And we really don’t have a good paradigm in which to treat it, because — how do you treat something that you don’t know the cause of?
In light of that, this is a statement from Joan Miller [MD], who is the Chief and Chair, Department of Ophthalmology, Massachusetts Eye and Ear, at her American Academy of Ophthalmology Jackson Memorial Lecture, 2012.
She stated, ‘It seems that AMD is a complex disease that results from the interaction of genetic susceptibility with aging and environmental factors.’
This sums up the orthodox, allopathic belief systems in medicine about macular degeneration, today. It’s a disease about aging, genetics, and then, environmental factors is a distant third and nutrition — or food — is way down the line.
Here’s another statement from a paper in 2001.
The authors wrote, ‘AMD prevalence was strongly age related.’
You can find this hundreds — thousands of times — in scientific papers about macular degeneration.
It’s believed that, ‘Well, we’re getting older and that’s what this disease is — uh — that’s a big part of what this disease is about.’
This is a paper from 2016 out of Bascom Palmer Eye Institute about genetics and AMD.
And the authors write this: ‘Currently, 52 gene variants… have been significantly associated with macular degeneration.’
Fifty-two!
And then, this: ‘The genetic component of AMD has been estimated at 45 to 70 percent.’
So up to 70 percent of this disease believed to be genetically driven.
In contrast to that, in 2013, I proffered this hypothesis — if only to myself.
It goes like this: The ‘Displacing Foods of Modern Commerce’ are the Primary and Proximate Cause of AMD.
I didn’t come out with this, publicly, until August of 2016, after extensive research.
The corollary to this is that ‘Any Ancestral Diet Will Prevent and May Treat AMD — Existing AMD.’
Alright, for those of you not aware, ‘Displacing Foods of Modern Commerce’ — just think of that as processed foods — and we’ll come back to that.
Just a week ago, our first scientific paper on this thesis came out last week in the journal, Medical Hypotheses.
My colleague, Marija Stojanoska [MSc], who is a nutrition researcher, and I have worked on this for years, and we’re very proud of this.
This is available through our website for free right now. Elsevier, the journal, has given us an author’s link, and you can download this from our website. I’ll give that at the end – and I’d love for you to read that if you’re interested.
Okay, now don’t let me lose you here. I’m just going to show you a little part of the retina, because I want you to think about the fact that macular degeneration shares a lot of analogies to heart disease.
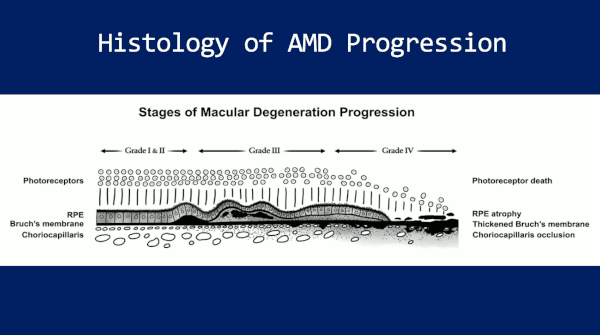
So this — it’s just part of the retina — the part that I really want you to think about. There’s the photoreceptors on top, which is these lollipop looking things, and those are the rods and cones. That’s what begins the ‘seeing’ process.
Deep to that is RPE — Retinal Pigment Epithelium. And then down at the bottom is Choriocapillaris, which is the vascular layer. That’s what brings – you know – vascular nutrition to the inner-retina.
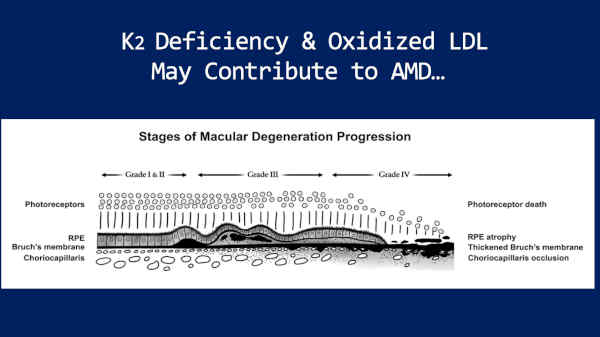
Now, sandwiched between RPE and Choriocapillaris is Bruch’s Membrane — this dark membrane, here.
And on the far left side, we have a very healthy macula and as you move to the right, this is a very diseased macula. This is representative of bad macular degeneration.
And what I want you to notice is that, what happens is that Bruch’s Membrane thickens with lipids and calcifies, much like an atherosclerotic plaque!
It behaves a lot like the intima layer of an artery — like a coronary artery — and then it becomes a barrier to the transmission of nutrients back and forth between this vascular layer, the choriocapillaris, and the RPE and the photoreceptors.
So what happens is — in the end result — is, these RPE cells die and each one of those RPE cells supports about 30 photoreceptors (rods and cones).
And so when the RPE cells die, the photoreceptors die.
And guess what? Neither of those are regenerative. So once they’re lost, they’re gone forever. Just think of ’em like brain.
So this is why we need to catch AMD as early as possible.
So keep in mind — lots of similarities, lots of analogies — to heart disease here.
Okay, treatment for dry macular degeneration. This is orthodox treatment today.
This is what ophthalmologists and optometrists agree on:
Synthetic vitamins called AREDS Formula. This is E, C, beta-carotene, zinc, and copper, and we’ll come back to this. Dark, leafy green vegetables, exercise, and we tell these people not to smoke.
Now, I agree with all of this, with the exception of the synthetic vitamins. Let me show you why.
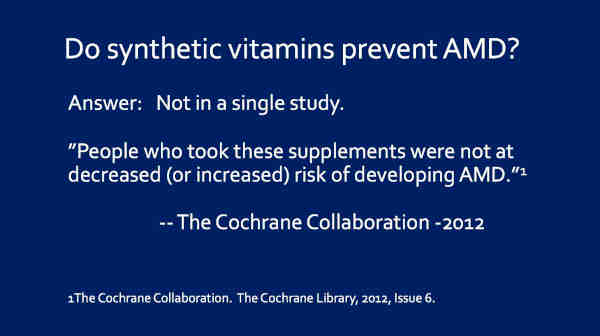
The first question to ask is, ‘Do these synthetic vitamins prevent macular degeneration?’
Anybody know?
(Participant: ‘No.’)
Thank you. No. Right. Not in a single study.
So the Cochrane Collaboration looked at this in 2012. There had been four studies; 62,520 people, randomized to synthetic vitamins – multivitamins – and Cochrane said this, ‘People who took these supplements were not at decreased (or increased) risk of developing AMD.’
So these vitamins don’t prevent the disease.
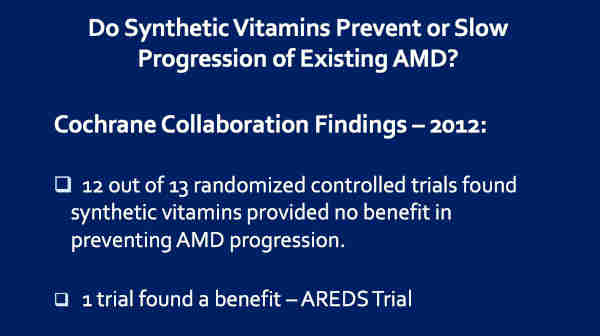
But do these vitamins prevent or slow progression of existing AMD?
So once we have it [AMD], do they benefit?
Well, once again, the Cochrane Collaboration comes to the rescue. They found, in 2012, there had been thirteen randomized, controlled clinical trials looking at whether or not these synthetic vitamins will help prevent progression of the disease, once you have it.
And, out of those thirteen, twelve of these trials, essentially, failed.
One trial found a benefit. So let’s — that trial is called the Age-Related Eye Disease Study [AREDS].
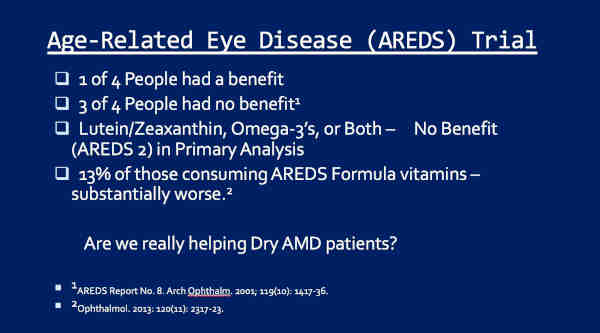
So let’s look at this AREDS trial.
In the AREDS trial, one of four people had a benefit when they got these vitamins: E, C, beta-carotene, zinc, and copper.
That means, three of four had no benefit. Right?
And then in AREDS 2, what they did, is they decided to add in lutein and zeaxanthin, because these are carotenoid pigments that accumulate in the macula, and you know, are thought to help protect the macula. And they most certainly probably do. So they added in either those or omega-3 fatty acids, or both, and then followed up people.
And guess what? Initially, they said, ‘No benefit,’ in the primary analysis.
Then they went back, looked at all the data again in a secondary analysis, and they said, ‘Nope, the lutein and zeaxanthin are of some benefit.’
Now, 2013 rolls around, and Carl Awh [MD] and colleagues, in Tennessee, looked at all this AREDS data in relation to genes. And what they found was that, uhm, a certain subset of patients that have what’s called ‘high CFH, low ARMS2 gene profiles,’ 13% of the total, were twice as bad off if they consumed the AREDS formula vitamins.
And then, things have gotten a little more muddy, since then. Now it looks like, possibly, 30% of patients will be worse off with the AREDS formula vitamins and about 60 or 70% are a little better.
So now there’s questions about genetic testing and treatment with these synthetic vitamins — and this is all very controversial. The NIH [National Institutes of Health] does not believe in testing. They believe that everybody benefits a little bit. So it’s very controversial.
But to me, the question is, ‘How much are we really helping these people?’ You know, one of four are better, 13% worse, or 30% better, 60% — I’m sorry — 30% worse, 60% a little bit better.
It’s not a very good outcome.
Alright, and then I want to raise this issue of a possible paradox with all this.
These synthetic multivitamins do not prevent AMD in any trial.
And yet, we expect them to prevent progression of existing disease!
I mean, just logically, does that make sense? I’m not saying it doesn’t. But, I just want to let you think about that — is there logic in that?
Okay, so let’s go back to this hypothesis —
The ‘Displacing Foods of Modern Commerce’ Are the Primary and Proximate Cause of AMD.
So where did I come up with this term ‘Displacing Foods of Modern Commerce’?
Anybody know that?
(Audience: Laughter, mentioning Weston A. Price)
Everybody here knows that, right? Okay.
From this man — Weston A. Price.
So I just learned about Weston A. Price last night, so I decided to include him in my talk…
(Audience laughter)
So you think I’m kidding?
(Audience, more laughter)
Okay, so for all of you Weston A. Price acolytes, like me, I have known Weston A. Price only since 2013. He changed my life. And so did the Weston A. Price Foundation, and thank Goodness for that.
So for all of you that are acolytes, bear with me. Let me go through five slides here to set the foundation for Price for those people that may not know.
Weston A. Price was a highly accomplished scientist, researcher, and dentist, who in the 1930s, spent the better part of that decade traveling the world, evaluating people on five continents, fourteen nations, hundreds of tribes and villages, thousands upon thousands of people, in attempt – really – to determine two things:
A) What it was about diets that kept people’s teeth healthy, and
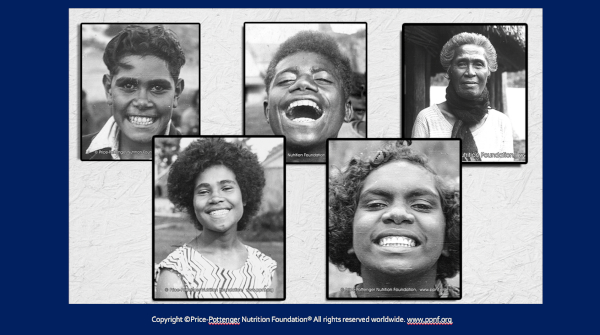
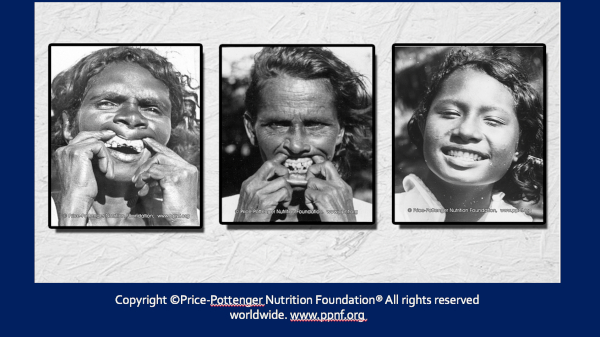
B) What it was about diets that kept people generally physically healthy, and then on the contrary, what led to dental decay and physical degenerative disease. Right? And what Price found, all over the world, on five continents, was people that looked like this!
People that are happy, healthy, vibrant, in extraordinary physical condition, and they had fantastically beautiful, straight, natural teeth, more than 99% cavity free, generally, and these people had immunity to our chronic, degenerative diseases.
They didn’t have heart disease, cancer, arthritis, type 2 diabetes, obesity — and they had immunity to infectious diseases like tuberculosis, again, as long as they consumed their native, traditional diets. But as soon as they began to consume what Price called, the ‘displacing foods of modern commerce,’ —
— which he defined, as refined white flour, sugar, canned goods, sweets, confectionary, and vegetable oils — when they began to consume these, the next thing that happened, of course, was dental decay.
Like these two ladies on the left.
And then this was followed by the degenerative diseases, like arthritis, cancer, loss of immunity to infections, right?
All three of these ladies are Australian Aboriginals. The two on the left were consuming the ‘displacing foods of modern commerce;’ the one on the far right continued her native, traditional, Aboriginal diet.
And if you amplify this scenario ten-thousand times, I think, you have Price’s work, in a nutshell.
Now, these ‘Primitive Diets’ — there’s dozens or hundreds of them, right?
And one thing we know today that so many people are concerned about is macro-nutrient ratios, right? Now Price didn’t directly address this, but what we know is that macro-nutrient ratios didn’t matter. High-fat, high-carb, low fat — none of that made any difference.
What mattered was nutrient-density. Micro-nutrient density — the density of vitamins and minerals, in the food, right?
And these were all diets of plant and animal origin — and they all contained ‘Sacred’ foods. ‘Sacred’ foods being like organ meats, liver, fish eggs — foods that were rich in fat-soluble vitamins, because as you know, the fat-soluble vitamins are not widely distributed in the food supply, and they’re so critical.
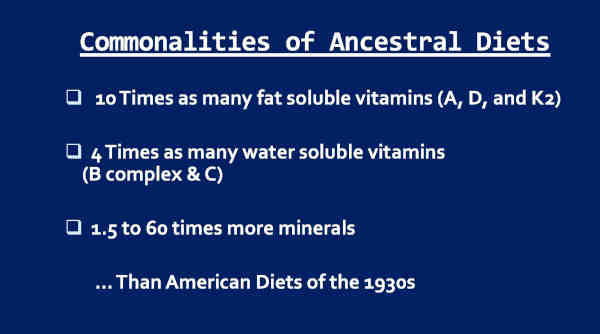
So Price sent back thousands and thousands of samples of these ‘primitive peoples” diets, for analysis, and what he found, of course, was that —
— these diets contained ten times as many fat-soluble vitamins, which is A, D, and K2, four times as many water-soluble vitamins, which is all the B-vitamins and C, and one-and-a-half to sixty times more minerals than did the American diets of his day, which was the 1930s. And you all know, we have far more processed food today, right?
So, alright. That wraps up the fundamentals of Price.
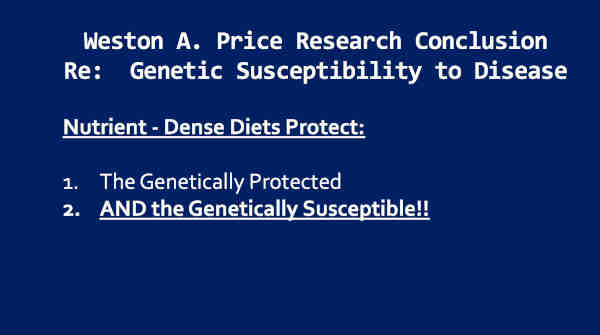
One thing I want to raise all of our attention to is this:
Price’s research — a conclusion from this, is that, in relation to genetic susceptibility, is that nutrient-dense diets protect the genetically protected, and they also protect the genetically susceptible, right?
Everybody has genetic susceptibilities to disease!
Women get more lung cancer when smoking the same amount of cigarettes for the same number of years, than men. Why? Genetic susceptibility.
But these nutrient-dense diets protected everyone. That’s a huge point, because macular degeneration — no question — has genetic susceptibilities.
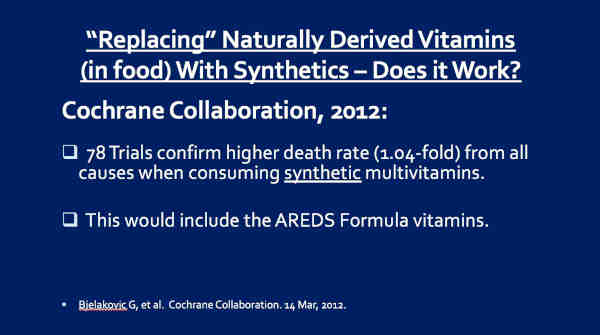
Alright, you know, since the 1940s, what we have believed is that — what people believe — not you in this room, but what people generally believe is that we can replace naturally derived vitamins with synthetic ones — and we can ‘fortify’ our foods, right?
And the question is, ‘Does this work?’
Once again, the Cochrane Collaboration looked at this in 2012. They analyzed 78 trials of people consuming synthetic multivitamins; confirmed a higher death rate from all causes when consuming these synthetic multivitamins. Relative risk 1.04-fold.
So if we consume multi-vitamins, we’re a little less healthy, and we die a little sooner.
This would include the AREDS formula vitamins. It’s another multi-vitamin.
Think about that.
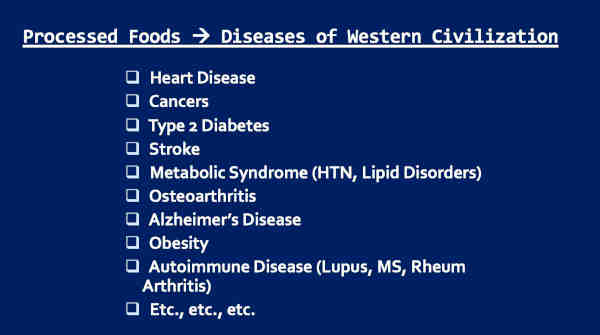
Alright, since Price’s day — Price died in 1948 — and since his day, there have literally been thousands of studies that have connected processed foods to ‘Diseases of Western civilization,’ right?
All these diseases: Heart disease, cancers, type 2 diabetes, stroke, metabolic syndrome, osteoarthritis, Alzheimer’s, obesity, autoimmune disorders — the list goes on and on.
I think that this very concept should be considered canonical theory, in medicine.
Canonical theory. All physicians in the entire planet should understand this concept. And my guess is — knowing the way I was trained, and the way most orthodox, allopathic physicians are trained — I don’t believe one percent of physicians knows this.
But this is fabulously important, as you know.
So, knowing that, in 2011 I understood that concept. In 2013, this finally hit me.
I asked myself this: ‘Could macular degeneration be another disease of western civilization?’ Might it be a disease that follows processed food consumption?
So let’s try to answer this.
So we’re going to go back to the risk factors for macular degeneration. Back to aging and genetics, right? This is what we believe.
But, what we also know is that macular degeneration is associated with heart disease, type 2 diabetes, metabolic syndrome, obesity — notice, I’m just listing ‘diseases of Western civilization,’ right?
And so, it occurred to me macular degeneration may just simply run with these diseases, because they’re all caused by the same thing.
But, we’ve got to go back to this question.
Could AMD be a disease of aging and genetics?
If so, then the prevalence of AMD in 1900 should be the same as in 1990, right? Or you can substitute your numbers, 1920 the same as 1970, unless you want to argue that our ‘genetic blueprint’ has changed, and I doubt anybody wants to argue that.
So, here’s the questions: Was AMD always so prevalent? And in fact, when could ophthalmologists even see the macula?
Late 2013, when I asked myself these questions, I had no idea — and so I went on a hunt — and this took months because this had not been investigated – uhh — until I found one very obscure paper long after I had done my complete investigation.
But, the answer is – is that — ophthalmologists could begin to see the macula in 1851, because of this man — Hermann von Helmholtz.
So von Helmholtz was a German born physician and physicist, who designed the ophthalmoscope — the device that we use to look into the back of the eye.
He published this design in a book in 1851 and so this technology spread around the world within a decade. So the ophthalmoscope was in use all around the world by the late 1850s.
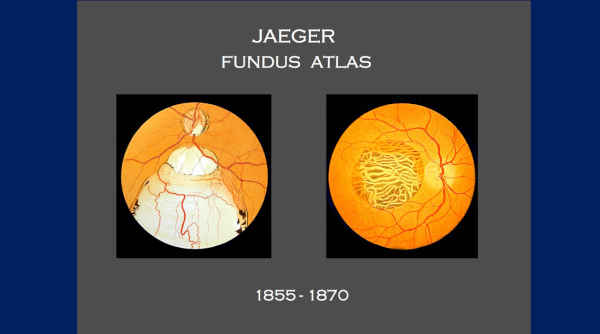
And ophthalmologists began to produce atlases of the retina that looked like this —
and of course, all of these atlases have the macula — it’s in the dead center! I mean, that’s what you’re looking right at when you look back there.
But guess what?
None of these images in the 19th century were of macular degeneration!
The most common condition of the retina today — and none of these images were of AMD.
Why?
Twenty-three years goes by, in fact, before this man, Jonathan Hutchinson, British ophthalmologist, London, England, described macular degeneration for the first time, in 1874. He describes four cases from his clinics he collects in Great Britain.
Another eleven years of silence — and then this man, German ophthalmologist, Otto Haab, discussed macular degeneration in a lecture, in 1885. He presented no cases.
Another decade goes by. Otto Haab publishes a paper in which he has evaluated 50,000 ophthalmic patient medical records, and determined that macular degeneration was as rare as traumatic maculopathy and myopic maculopathy. These are extremely rare disorders! I saw a handful of these in 24 years of practice — and I would see that many macular degeneration patients every day, at least, often in a half-a-day.
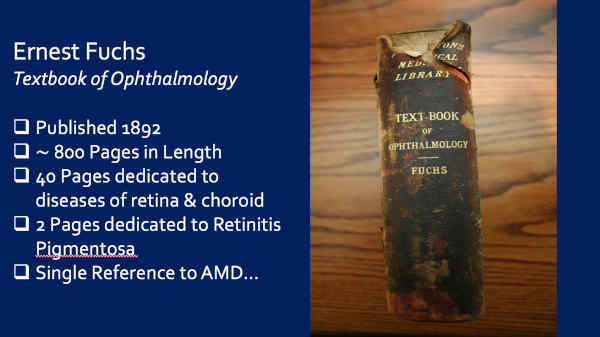
Ernest Fuchs published this textbook of ophthalmology, in 1892, in English.
This is my original copy, from 1892. It is 800 pages in length. He dedicated 40 pages to diseases of the retina and choroid, and they are very extensively and meticulously reviewed. He dedicated two pages to the condition of Retinititis Pigmentosa — a retinal condition that affects 1 in 4000 people.
But, he made only a single reference to macular degeneration — this —
It read, ‘Finally, a disease of the macula is observed in old people, which usually affects both eyes about equally, and is referable to senile changes.’
Eight-hundred page book — one sentence — almost a footnote.
Another of the most prominent names in all of ophthalmic history — Julius Hirschberg — published this book by the name of The History of Ophthalmology — The First & Second Half of the 19th Century.
This book came out in 1914-1915 and despite its name, he reviewed ophthalmic history all the way up through 1914.
Three-hundred-and-fifty pages in length — he made not a single mention of macular degeneration.
But you might be thinking that, ‘Well maybe ophthalmologists weren’t using the ophthalmoscopes, right? Maybe they weren’t looking back there all the time.’
Well, these two ophthalmologists, Landolt and Snellen, began collecting ophthalmoscopes in the 1860s. By 1880, they had collected 86 different versions of ophthalmoscope. Light bulbs were added in 1886.
By 1901, in Atlantic City, New Jersey, they had on display 140 models of ophthalmoscope, at the 50th anniversary of Helmholtz’ invention.
And by 1913, Landolt had collected 200 models of ophthalmoscope in use around the world. These are different brands and models.
So the people that want to argue, ‘Well, they weren’t using them…’
Well, first of all, they haven’t read all the books that shows [sic] that they extensively reviewed the retina. And secondly, this would be like saying, ‘Well, there was 200 models of cars being produced that year, but nobody ever drove ’em.’
Right? I mean, that would be the way I would think about it.
So, and then this — in 1889, Fuchs’ textbook, which was originally in German, uhm — he reviewed that there were six dilating agents in use at that time. In fact, they — so by the 1880s, they’re dilating eyes with six different dilating agents.
Alright, this slide is going to address this ridiculous old canard that, ‘Well, we just didn’t live long enough to get these diseases.’
(Audience laughter)
Awe, I love that you guys laugh at that, because this drives me crazy!
Uhm so, alright.
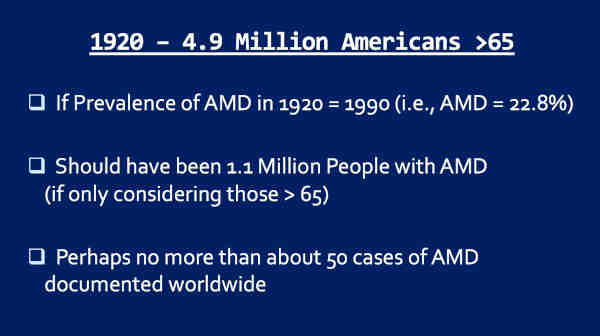
In 1920, there was 4.9 million Americans on Social Security. Anyone can go to the internet and look this up, like I did. So they were over the age of 65, right?
And if the prevalence of macular degeneration in 1920 was the same as in 1990, which was 22.8%, there should have been 1.1 million people with macular degeneration, if we only look at those over the age of 65. And yet, perhaps no more than 50 cases of macular degeneration in all the world’s literature.
1927, this man enters the picture — Sir Stewart Duke-Elder.
So Duke-Elder was a British ophthalmologist — London, England. He would become the most dominant force in ophthalmology from the 1920s to the 1960s, at least in the English language.
1927 he publishes this textbook, called Recent Advances in Ophthalmology.
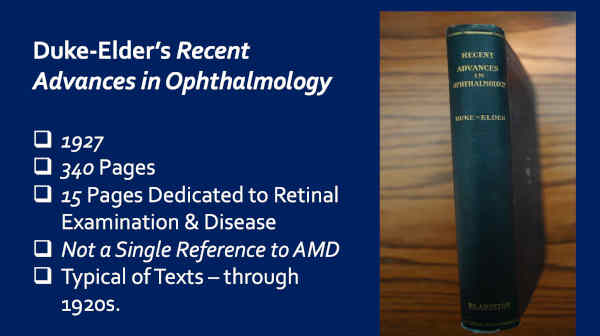
Again, this is my copy — original copy. It’s 340 pages in length. He dedicated 15 pages to retinal examination and disease.
Again, not a single reference to macular degeneration, which is typical of textbooks of that era.
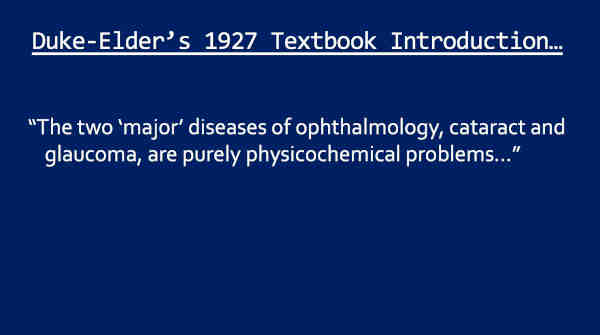
In fact, in the opening, he writes this — wrote this…
‘The two ‘major’ diseases of ophthalmology, cataract and glaucoma, are purely physicochemical problems…’ and he continues.
Today, the two ‘major disease’ of ophthalmology would be cataract and macular degeneration. But he makes no mention of macular degeneration – 1927.
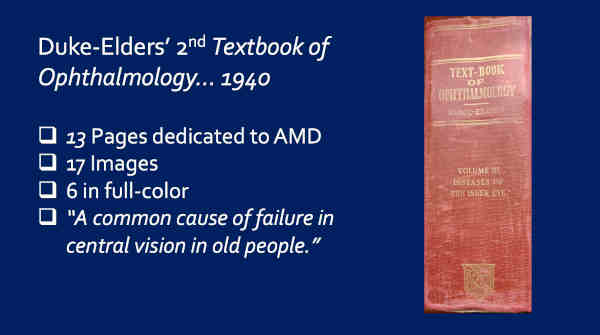
Thirteen years later, however, he publishes this textbook —
— And this is my copy. In this textbook, in 1940, he dedicates 13 pages to the condition of macular degeneration, 17 images, six of which are in full-color, and he calls macular degeneration ‘A common cause of failure in central vision in old people.’ That’s a quote.
So in the 1920s, I don’t believe he even knew what macular degeneration was!
He didn’t mention it in his comprehensive textbook of ophthalmology. But by 1940 it was becoming a common condition.
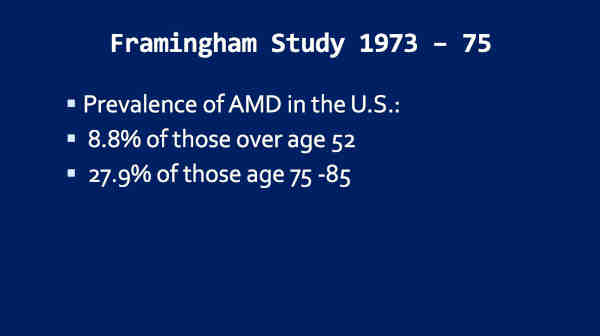
So let’s jump ahead to 1973-’75, the Framingham Study — now shows that 8.8% of those over the age of 52 now have AMD —
— 27.9% of those over the age of 75 have the disease. Now we have an epidemic. This is over 4 million Americans affected with a condition that wasn’t worth mentioning in any textbook or paper of ophthalmology, for the most part, 48 years earlier.
If we look over at the UK, Jennifer Evans and Richard Wormald did this research.
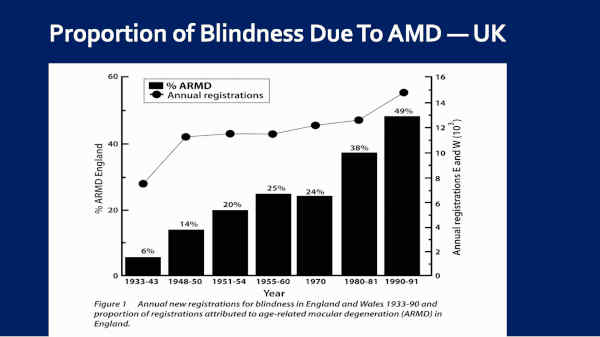
They looked at macular degeneration as a cause of blindness in the U.K., because it is registrable there, with the government. And they found that, as you can see here, 1933 to 1943, 6% of blindness was due to macular degeneration. That jumped to 24% by 1970, 49% by 1990, and by 2014, 56 percent.
So we went from 6% [blindness secondary to AMD] in the late 1930s to 56% by 2014.
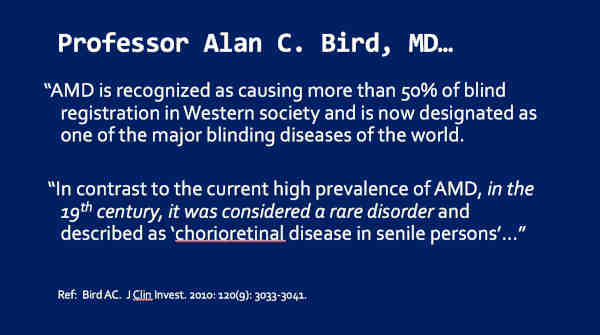
Professor Alan Bird, of Moorfields Hospital in London, probably the most published ophthalmologist of the last several decades, in 2010, wrote this, in a paper:
‘AMD is recognized as causing more than 50% of blind registration in Western society and is now designated as one of the major blinding diseases of the world.
‘In contrast to the current high prevalence of AMD, in the 19th century, it was considered a rare disorder and described as ‘chorioretinal disease in senile persons.”
He continued —
‘There is evidence that the current increased prevalence of AMD cannot be fully explained by increased life expectancy. Furthermore, the disease is now recognized as a burden in societies in which it was rare 30 years ago.’
The societies he was talking about — because this was 2010 — the societies he was talking about where it [AMD] was rare 30 years ago, was (sic) Japan and India. And I’m going to show you Japan shortly, and this is absolutely correct.
So I would submit to you that the – the prevalence of AMD is increasing — and increasing dramatically.
And the question is, ‘Why? What induced this?’
Well, you know where I’m going with it, right?
Okay, so let’s talk about the U.S. diet, because it – you know – we set the stage for the entire world, really, on this. Didn’t we?
Four processed, nutrient-deficient foods have changed the world’s diets forever, right?
Refined sugar, refined white flour, polyunsaturated vegetable oils [PUFA], and trans fats. Just look at these briefly with me.
So, sugar — how many of you have seen Robert Lustig’s presentation called, “Sugar – the Bitter Truth”? Have any of you seen that? It’s a lecture — it’s on YouTube – 2009. It’s a really excellent eye-opener as was his book Fat Chance that came out in 2011.
But, if we look historically, from the 16th through the 19th centuries, we wouldn’t have had sugar in any significant quantities at all if it weren’t for this egregious, regrettable part of our past, and that’s the slave trade.
But my point to you today is that sugar was such a valuable commodity from the 16th through the 19th centuries that it was often shipped to the U.S. under lock and key — right up through the mid-19th century.
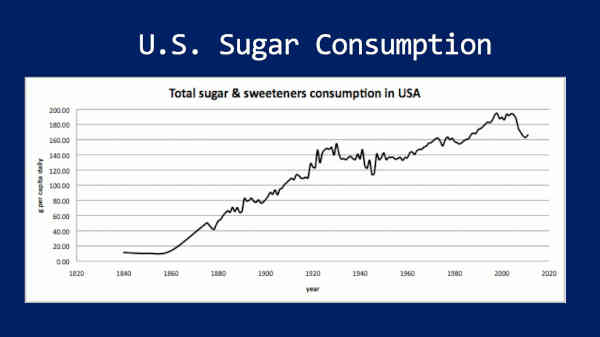
And so this is our data from 18— uhm, sugar consumption from 1840 to the present, essentially, in the U.S. But, let me just mention Stephan Guyenet’s research because I love his findings. They were able to go clear back to 1822 when, in the U.S., we consumed six pounds of sugar per person per year — and that rose to nearly 108 pounds per person per year by 1999 — a 17-fold increase in sugar consumption during that period.
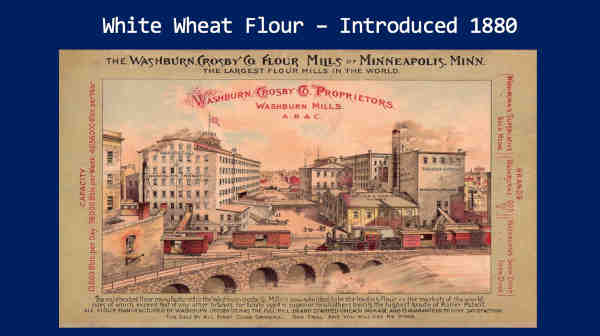
Next — white wheat flour.
Introduced in 1880. Why? Because that was the year that we got roller-mill technology around the world. In fact, it was introduced right here in Minneapolis, Minnesota with the Washburn Mills — and this is a picture of those mills.
Well, these mills were roller mill technology. Up through all of history, wheat was ground on stone mills. Stone mills would always produce a whole grain flour.
And so the roller mill could shear away the bran and the germ, which would effectively remove B-vitamins, E-vitamins, fiber, minerals, omega-3, and omega-6 fatty acids — and produce this very fine – you know – refined white flour, which is what the people wanted. But it’s a nutrient-deficient food.
And today, 20% of the world’s diet is wheat. And at least in the U.S., 85.3% of this is refined, white flour. Loren Cordain’s group showed this a few years ago.
Okay, third — vegetable oils — also introduced right around 1880, with cottonseed oil.
So manufacturers determined way back then that they could take cotton seeds, which were a waste product, crush them, heat them, run them through a hydraulic press —
— and then they go to this oil extraction, which is a petroleum-derived hexane solvent bath, right?
Then they go to the refining stage, which they’re alkalinized, bleached, and deodorized — all chemically, right?
And then we have the ‘edible oil,’ that they tell us is so great for us to eat.
So, one of the things that happened is that, as this article from the Atlantic — from 2012 shows — is that vegetable oils replaced animal fats.
And one of the things that you’ll notice in the sub-title is that these cheap, factory-made oils are loaded with trans-fats, and I’ll come back and show you this, shortly.
We’re going to look at what’s wrong with these.
And I want to mention this. This is, uh-uh — a quote out of Popular Science in reference to cotton seed.
They said, quote, ‘What was garbage in 1860 was fertilizer in 1870, cattle feed in 1880, and table food and many things else in 1890.’
Cotton seed — a waste product — became our food!
Then, 1900 — Valerius Anderson invented this — the continuously operated expeller press.
This was the first step in the ‘Edible Oil Industry.’
Because this could crush seeds and start to produce that oil. Now this wasn’t — and then the next step, of course, was the all the chemical refining that they did.
So today, you know most Americans don’t think a thing of grocery store isles lined with all these vegetable oils. They don’t question the health risks of these.
Does anybody know what this is?
(Crowd inaudible murmurings)
Oil refinery. A vegetable oil refinery!
(Crowd: ‘Wow!’)
That’s what I thought! I thought these were petroleum refineries!
So why are they so big?
Because they’re producing 24% of the American food supply — and probably something approaching that in most developed nations.
Almost a fourth of our ‘food’ is coming out of these ‘kitchens.’ Looks like your kitchen, right?
(Crowd laughter)
I just think this — if anybody ever went in there and saw what happens to these oils — I don’t think anybody would ever eat that — eat those oils again.
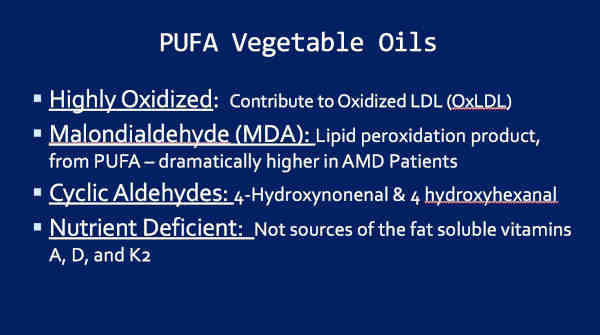
So the PUFA vegetable oils — highly oxidized. These are very dangerously oxidized substances and this contributes to oxidized LDL.
Low-density-lipoprotein [LDL] was never bad, until it became oxidized. How does it become oxidized? PUFA vegetable oils attach. They’re, as you know, now they’re extremely fragile. They oxidize easily. In fact, these are oxidized by the time they ever hit the bottle and then, if you cook with them, and metabolize them, they oxidize further.
This begins the whole process of atherosclerosis.
Second, malondialdehyde [MDA], a lipid peroxidation product that comes out of these, from these PUFAs, is dramatically higher in macular degeneration patients.
Third, these contain cyclic aldehydes — 4-hydroxynonenal and 4-hydroxyhexanal. I wish I had time to go into this, but these are extremely dangerous substances!
And finally, these vegetable oils are nutrient-deficient. They don’t contain the fat-soluble vitamins, A, D, and K2, that the animal fats would.
I like what Cate Shanahan said — was this: ‘Nature doesn’t make bad fats. Factories do.’
Most of these oils coming out of plants are not bad on their own. It’s when they go through these factories.
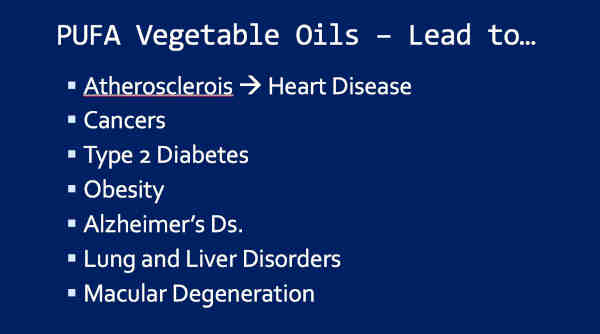
So the PUFA vegetable oils lead to all of this disease, right?
Atherosclerosis, heart disease, cancers, type 2 diabetes, obesity, Alzheimer’s, lung and liver disorders, macular degeneration — honestly, this list could go on much further. I just ran out of room, right?
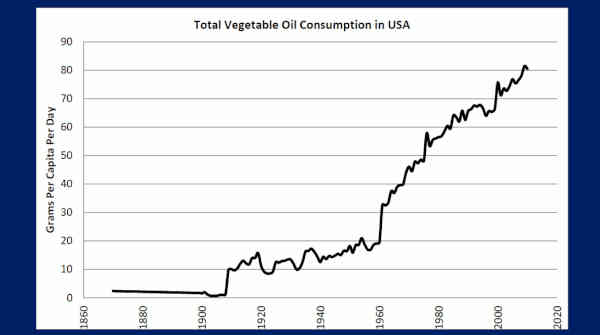
And so – and this is our data from our research. This is vegetable oil consumption in the U.S.
And you can see here, that from 1880 until 1909, we consumed about 2 grams a day and then that gradually elevated all the way up to 80 grams a day! Per person, per day, by 2012.
Eighty grams — at 9 calories a gram, that’s 720 calories worth — per person!
Now, in 1900, way back here, 99% of our added fats were animal fats — lard, butter, and beef tallow. By 2005, 86% of our added fats were vegetable oils.
These almost completely supplanted the healthy animal fats.
And, of course, back here in 1900, we had no heart disease and we had no macular degeneration. They were both extreme medical rarities.
So what do we do with them?
Well, we can run our cars on these vegetable oils.
(Crowd laughter)
I’m not kidding ya! This is the world’s first vegetable oil Smart Car! I think this is smart!
They can actually run on left-over vegetable oils. The problem is — is right now, there’s not enough vegetable oils to run these. But diesel engines will run on these. They simply have to heat the oil first.
And so, uhm — take a look at this article — out of CNN.
‘Can vegetable-oil cars save the world?’ I mean, this is actually serious!
This is what we should be doing with these — is — we should be running our cars on ’em. They’ll even suffice as motor oil. Doesn’t seem like we ought to be eating those, does it?
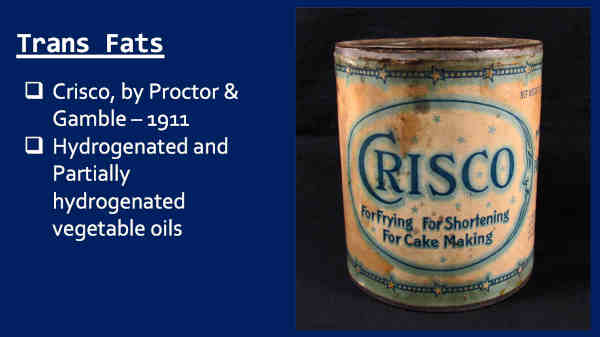
Okay, so fourth — nutrient-deficient, processed, man-made ‘food,’ and this is probably about the worst — trans fats.
Introduced by Proctor & Gamble in 1911 — Crisco — right?
Hydrogenated and partially hydrogenated vegetable oils.
Uhm, so Proctor & Gamble marketed these with ads like this:
‘Crisco — Better than butter for cooking,’ right?
This is what they did — they moved in on butter and lard, because they were cheaper. And they convinced housewives that this is the way to cook — that this is the healthier way to go.
In fact, this is my favorite ad of theirs —
‘Crisco — 3 Sure Ways to a Man’s Heart!’ (Crowd laughter)
Yeah, if you want to kill him! (Crowd laughter)
And you’ll never be charged with murder! (Crowd laughter)
Or you could give him Alzheimer’s. So it depends on your motives — your goals, right? Depends on what your goals are.
Alright, so trans fats are associated with —
Heart disease, cancers, type 2 diabetes, Alzheimer’s, depression, infertility in women, obesity, and macular degeneration.
Notice this list is really similar to the PUFA vegetable oils.
But these trans fats have been banned, right?
The FDA removed these from GRAS status — Generally Regarded As Safe status — June 16, 2015. Three years for manufacturers to get these out of our food supply. Right?
So June 16th, 2018, these should no longer be in our food supply, right?
Wrong. You know why?
Because PUFA vegetable oils contain up to 4.6% trans fats. In fact, 1.1% of vegetable oils are trans fats, on average!
So, the FDA has not ruled on this.
But these are big carriers, given our 80 gram a day consumption of trans fats. [Note: Mis-speak per Dr. Knobbe; should have been 80 gram a day consumption of vegetable oils.]
So, while we’re here. Ten studies have correlated an increasing risk of AMD development or progression to increasing vegetable oil and/or trans fat consumption. And this is before our research.
And I’m coming up to that.
So big picture — back to the big picture here.
This is straight from the USDA — 2009 — 63% of our food is coming out of those four things — added vegetable oils, trans fats, sugar, and refined grains.
I find it very interesting that this comes right out of our own USDA. You know why that is? Because they recognize that this is such a huge problem. They know it. Somebody there knows it.
So, don’t you wish that foods were labeled like they should be? (Crowd laughter)
I recommend staying away from that ‘Heart Disease Spread.’
Alright, so — moving on.
Now I’m going to talk about the fact that AMD follows processed food consumption, worldwide.
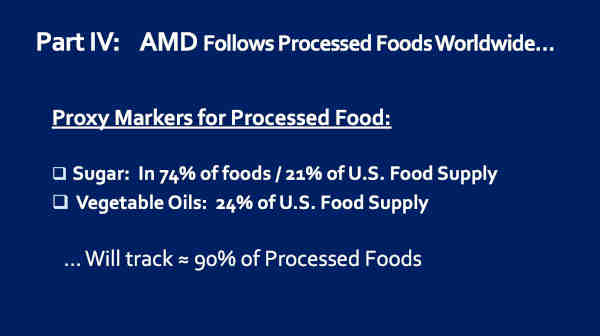
So what we did in our research — Marija Stojanoska [MSc, Nutrition Researcher] and I — is that we tracked proxy markers for processed food. We used two markers.
Sugar, because it’s in 74% of the 600,000 food items available in the U.S. and it’s 21% of the American food supply.
Second, vegetable oils. Why? Because they’re — as I’ve mentioned — 24% of our food supply.
So these two man-made, processed foods are 45% of American food consumption. But they will track, we believe, around 90% of all processed foods.
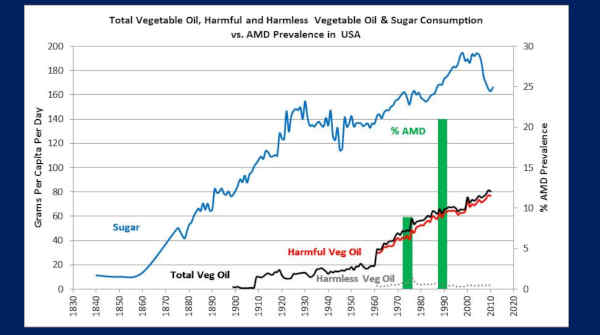
So let’s see what happens when we track these.
So this is the United States, going clear back to 1840 with sugar, in the blue, okay and then, total vegetable oils down here in the black, split out as what we called ‘harmful vegetable oils’ — now these are the ones containing the PUFA’s — alright?
And then in the green bars is macular degeneration prevalence.
Now what I want you to notice, is that back here in 1900, remember, we didn’t have any macular degeneration? Extraordinary medical rarity!
And remember, by the 1930s, we were starting to see AMD. Somewhere in here [pointing to 1930s on the graph].
And by the 1960s or ’70’s, for sure, we were at epidemic proportions [of AMD].
So the point of this is that consuming these foods for 30 to 50 years or so, leads to macular degeneration. We have data in 25 nations that supports this.
So I’m just going to show you a few samplings of this, today.
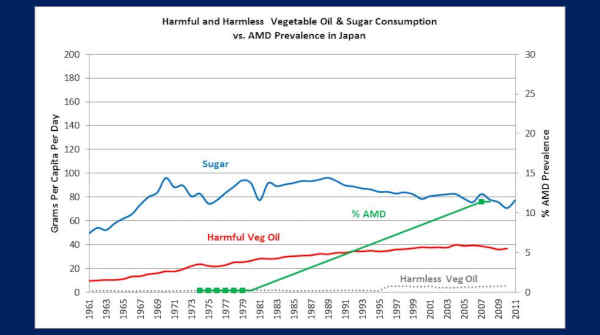
The next one is Japan — and this is the quintessential nation to illustrate this whole point.
So take a look at their sugar consumption. It was at right around 50 grams a day back in 1961 and elevated to 80 to 90-some grams a day in succeeding decades. And then their PUFA vegetable oils — the harmful oils — were at 9 grams a day in 1961, elevated to 40 grams a day by 2003.
Now look at their AMD prevalence — in the green — 0.2% from 1974 to 1979, elevated to 11.4% by 2007.
That’s a 57-fold increase in the prevalence of macular degeneration, in 30 years.
That cannot possibly be explained by aging or genetics.
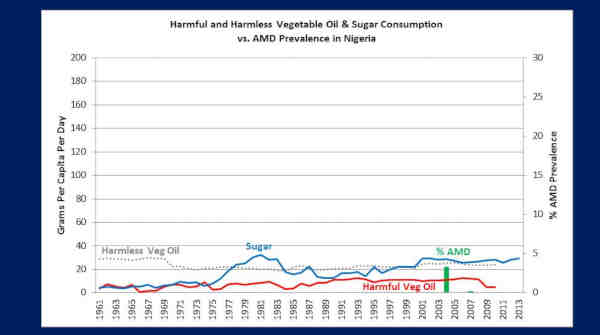
This is Nigeria. Now you’re going to notice that, — so, this is an entirely African population — and you’re going to notice their sugar consumption and PUFA vegetable oil consumption is extremely low.
They’re down here around — averaging around 15 grams a day, since 1961. And – uhm — and here’s their AMD prevalence — 3.2%. Right? Over here.
Three-point-two [3.2] percent, in 2004.
So, now this pales in comparison to our 22.8%, right? And it should because we consume far more processed foods than they do, as evidenced by our sugar and vegetable oil consumption.
But, this 3.2% — this was in Onitsha, Nigeria, which is a metropolitan population of 1.1 million people. Guess what they have access to there?
(Crowd: ‘Grocery stores… Processed food’)
Yeah, grocery stores — processed food. Fast food.
Okay, now look at this little tiny blip over here, in 2007. Uhm — right over there [pointing at the graph].
That represents a prevalence of AMD of 0.1%.
This was in Southwestern rural Nigeria. Guess what they don’t have access to there?
Grocery stores — right. They can’t get processed food there — they’re consuming a native, traditional diet!
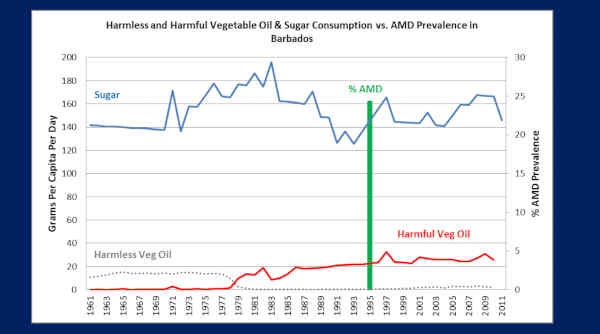
So keep in mind this 0.1% prevalence of AMD, in this African population of Southwestern rural Nigeria, when we look at this next population, of Barbados.
So Barbados, down in the Caribbean, is — their heritage is almost – nearly 100% West African. And, in this study, this is a 97% African population.
Now, nutrition researchers all over the world know that Barbados is a mecca for processed food. It is known for this. They import almost all of their food, like Greenland, and we all know that when you import the food, it’s all nutrient-deficient, processed food.
So, now you can tell because — look at their sugar consumption — 140 to 180 grams a day — more than four times the World Health Organization’s recommendations.
Their PUFA vegetable oils down here in the red — headed towards around 20 grams a day in the late ’70s, uhm – and has been since, but they’re probably undervalued, because not all of these oil companies are reporting.
Now, to go with all their processed food though, they have, according to nutrition researchers, a ‘world profile of metabolic disease.’ So, metabolic syndrome, type 2 diabetes, obesity, heart disease, all of that, right?
Well, of course they would!
So now look at their macular degeneration — 24.3%!
Two-hundred-and-forty-three (243) times greater than the Africans of Southwestern rural Nigeria, who can’t get processed food.
Would anybody want to argue that this is about genetics, or aging?
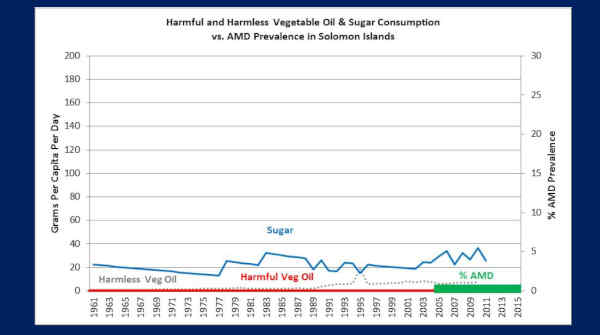
Okay, this is the Solomon Islands, in the South Pacific. This is a population of 630,000 people. They have three ophthalmologists to care for this gigantic population.
Look at their sugar consumption, from 1961 — hovering around 20 grams a day.
Look at their harmful vegetable oils — the PUFA’s — ZERO! They don’t get them!
And now look at their macular degeneration. From 2005 to 2015 — 0.2%!
So the U.S. has 74-fold more AMD, on average, than the Solomon Islands. And you can see the difference — sugar and vegetable oils — processed foods.
So these three ophthalmologists, they collectively averaged seeing one AMD patient every two months — each one of them — over the last ten years.
Most American ophthalmologists see an AMD patient, probably about every hour or so. And a lot of them will see 20 to 40 AMD patients a day — the retina doctors.
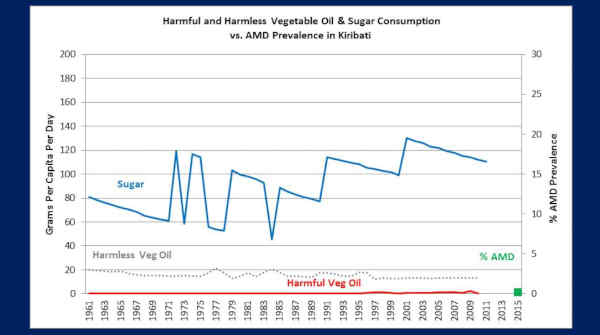
Okay, the last nation we’ll look at — Kiribati.
So Kiribati is an island nation, 1200 miles directly south of Hawaii, the population is about 113,000 people. They have one ophthalmologist for this entire population.
I point that out, because in the United States, there’s about one ophthalmologist for every 20,000 people. So they have one ophthalmologist for 113,000 people.
Now take a look at their sugar consumption — it’s been bouncing around — 80 up to 100-and-some grams a day, since 1961.
Uhm, but their harmful vegetable oils, like Solomon Islands — zero. They’re not getting them down there, because the companies don’t want to sell them down there. It’s too far to get down there and they don’t make any significant profit.
But this is not— isn’t totally reflective — these people are living mostly off of a native, traditional diet — lots of fish, lots of root vegetables, and mostly coconut oil.
Okay, so now look at their AMD. 2015 — 0.2%. This little tiny green spot [pointing to the graph].
Their ophthalmologist, Rabebe Takeraoi, 2015, saw two patients with macular degeneration, for the year!
Two patients for the year. And you can see the difference. Here, they’re on a — well mostly — a native, traditional diet, uhm with the exception of their sugar, uhm — and they don’t get vegetable oils.
Okay, now — but an issue a lot of people have raised to me is, ‘Well but these ancestral diets have lots of saturated fat. This is a problem, right?’ they say.
What are we going to do about this?
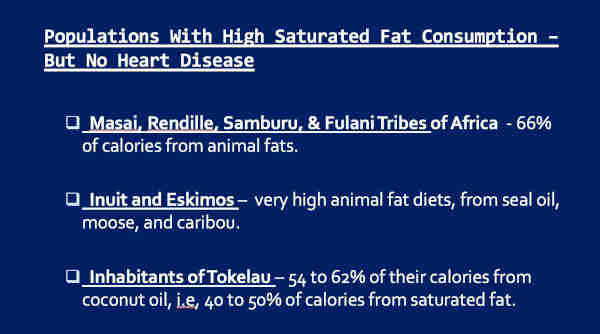
Alright, so here are some populations with high saturated fat consumption, but no heart disease. Many of you may already know this.
But, in Africa, the Maasai, Rendille, Samburu, and Fulani tribes — they are pastoralists. They consume mostly the meat, milk, and blood of the cattle they herd. Sixty-six percent [66%] of their calories coming from animal fat!
Close to half of that would be saturated. So around — their diet is around 30% saturated fat.
Our American heart association, even in 2017, says, ‘Don’t consume more than 5 or 6% saturated fat, right? ‘Oh you can have an egg every three days.’ Right?
And the Inuit and Eskimos, traditionally, very high animal fat diets! As you know, they dipped everything in seal oil — you know, they dipped their fish in seal oil all the time. They went after the fatted moose and caribou. They wanted the fat. Very healthy. No heart disease.
The inhabitants of Tokelau, in the South Pacific — this is a small population, but their consumption of coconut oil — 54 to 62% of their calories — and coconut oil is really high in saturated fat. So that means they’re consuming around 40 to 50% of their calories from saturated fat! More saturated fat than any population known on the planet, and yet they have no heart disease and they’re fantastically healthy people.
Well, suppose that’s not enough…
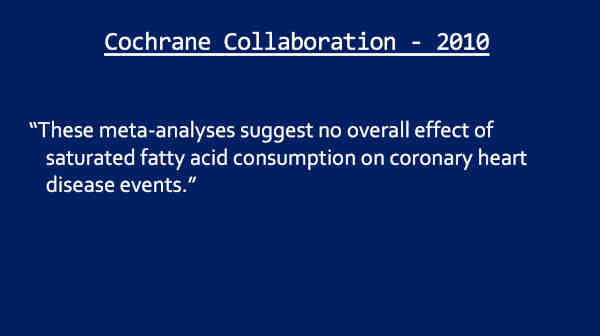
The Cochrane Collaboration, in 2010, looked at all the research on heart disease — saturated fat versus polyunsaturated fat. Well they said this, ‘These meta-analyses suggest no overall effect of saturated fatty acid consumption on coronary heart disease events.’
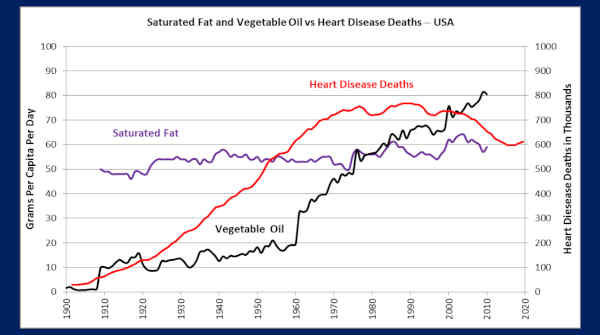
This is our data, which I think you will find interesting — because we already had the data looking at macular degeneration, so this is saturated fat, plotted against vegetable oils and heart disease deaths in the U.S. going clear back to right around 1909 is our oldest, or most recent data.
But you can see saturated fat consumption is practically a flat line since 1909, but look at the — look at the correlation between vegetable oils and heart disease deaths! I would say that’s remarkable, wouldn’t you?
I don’t know how anybody could look at this and say, ‘Nope, it’s saturated fat — that’s what’s killing us.’ (Crowd laughter)
How could you look at that, and conclude that?
Okay, next part. We’re at the second to last part here.
Fat-soluble vitamin deficiencies and macular degeneration —
So — we’re going to start first — because I think two fat-soluble vitamins — I mean, actually all three of them — we’ve got good data on two of them.
Let’s start with vitamin D.
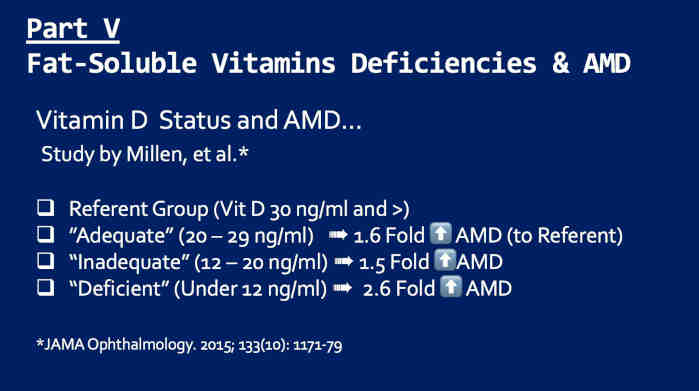
This is a study by Millen and colleagues. They looked at vitamin D status versus macular degeneration risk. So they call the ‘Referent Group’ to have a vitamin D of 30 ng/ml and higher — and I think that’s a good level for vitamin D.
They compared that to the ‘Adequate’ group at 20 to 29 ng/ml, and those people already had a 1.6-fold increased risk of AMD.
Then at the ‘Inadequate’ category, which is the next level down, a 1.5-fold increased risk of AMD.
And at the ‘Deficient’ category, under 12 ng/ml, a 2.6-fold increased risk of AMD.
So there’s almost a linear correlation between lower vitamin D status and higher AMD risk.
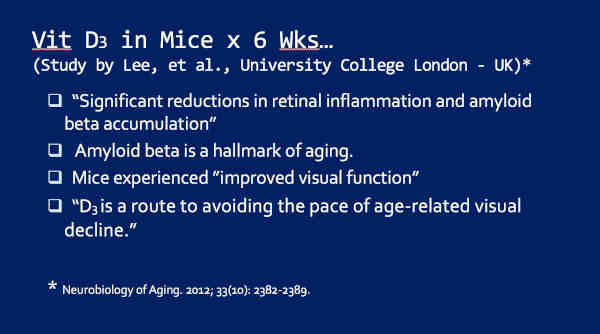
These researchers at the University College London, in the U.K. — they gave vitamin D to mice and then analyzed their eyes. And here’s what they found — these are quotes:
‘Significant reductions in retinal inflammation and amyloid beta accumulation.’
So amyloid beta is a hallmark of aging. It — it presents in Alzheimer’s patients, in their brains, and it presents in the macula.
They said these mice experienced, ‘improved visual function.’
These mice — they were reading more books, they were driving more cars — (Audience laughter) — they could run around at night better. They loved it!
Okay seriously, and they said, ‘D3 is a route to avoiding the pace of age-related visual decline.’ That’s a pretty powerful statement — just for D3 alone. Just this one thing alone.
Okay finally, there’s been four more studies that have correlated an inverse relationship between vitamin D and AMD.
So higher vitamin D — lower AMD risk.
So where can we get vitamin D?
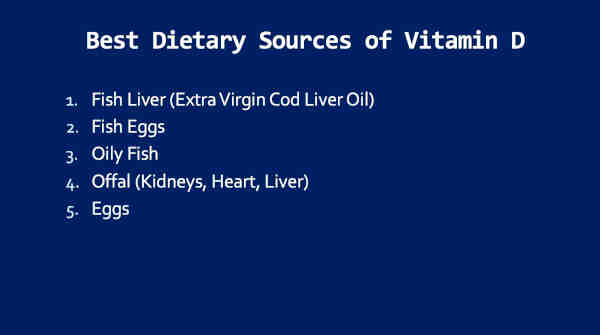
Fish liver — is one of the best sources there is. I really like extra virgin cod liver oil [EVCLO] — uhm — just because it’s cold-processed, and there are a few other reasons.
Fish eggs — Weston Price showed an excellent source of vitamin D and Sally Fallon-Morell’s group has also looked at this. I don’t remember the numbers, exactly, but fish eggs are a fantastic source. So — fish roe. If you eat sushi, it’s fantastic.
Other good sources — oily fish, [ recording malfunction: Dr. Knobbe continued, “offal, which is kidneys, heart, liver etc., organ meats, and eggs.”]
Okay, so moving on to vitamin A deficiency and macular degeneration.
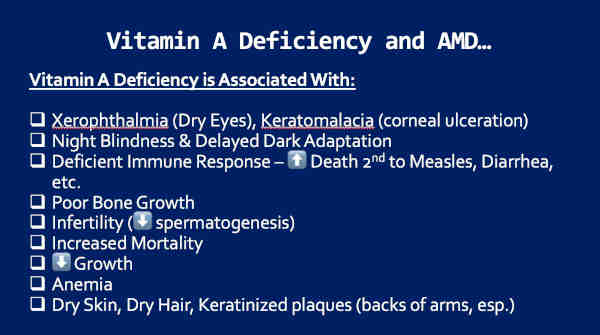
So vitamin A deficiency is associated with a lot of ophthalmic findings. Number one: Xerophthalmia — dry eyes. And in the worst case scenario — keratomalacia — which is corneal ulceration and this can be blinding.
Also leads to night blindness and delayed dark adaptation, which is that ability — you know — to dark adapt as you go from, you know, a dark — I mean, a light area, to a dark area, like a movie theatre.
It’s associated with a deficient immune response, poor bone growth, infertility, increased mortality, poor growth in general, anemia, and dry skin, dry hair, and so forth.
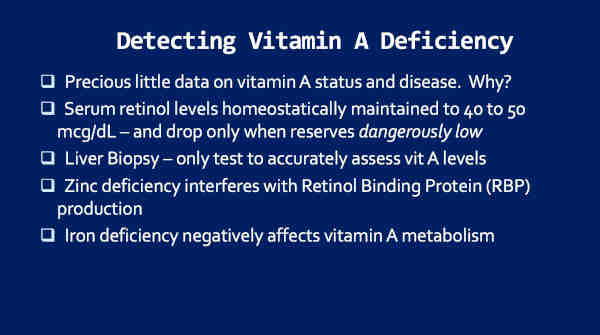
So why is it that we don’t have hardly any data on vitamin A deficiency and disease?
Well, the answer is — because serum retinol, the active form of vitamin A, is homeostatically maintained to 40 to 50 micrograms/deciliter [mcg/dl] and drops only when our vitamin A reserves are dangerously low.
How do we detect that? Liver biopsy! So to do that, you have to put, you know, plunge a big-core needle into your right upper-quadrant, into your liver, take out a chunk of your liver, and analyze that. Nobody will do this just to assess vitamin A status, for good reasons. Right?
A couple other things: Zinc deficiency can masquerade as a vitamin A deficiency, and so does iron deficiency. Alright?
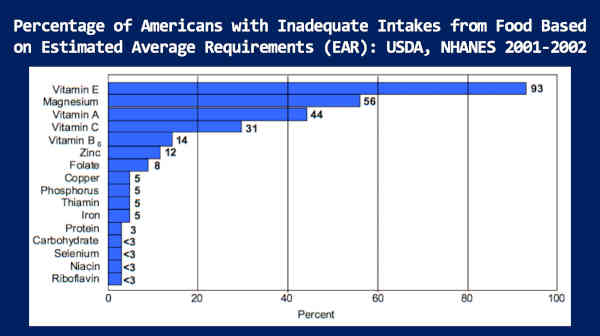
This is data from our own NHANES study. This is the percentage of Americans with inadequate intakes from food, based on the estimated average requirements [EAR].
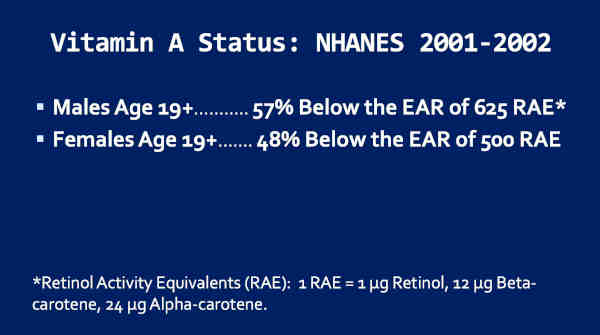
And, if you look at the third one down, you’ll see that the vitamin A — 44% of Americans are deemed to be vitamin A deficient, in terms of food intake, by our own Institute of Medicine.
And if we look only at adults — males age 19 and above — 57% below the estimated average requirement, and females, age 19 and above — 48% below the estimated average requirement.
Well, the Institute of Medicine’s standards, for what’s required, would probably be 10-fold lower than what Weston A. Price would have set them at, right?
And so I would estimate that nearly 100% of Americans are already vitamin A deficient.
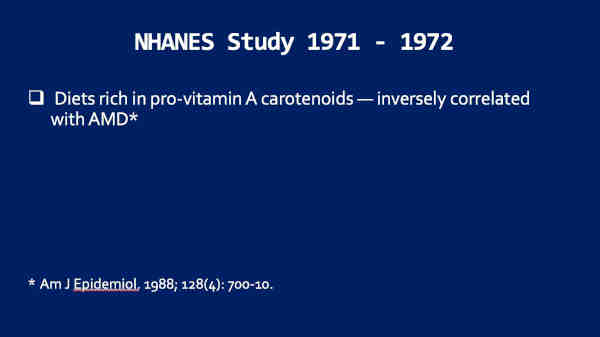
In fact, if we go back to the NHANES study of 1971-1972, diets rich in pro-vitamin A carotenoids were found to be inversely correlated to macular degeneration.
So let’s look at these vitamin — a couple of vitamin A studies — relating to delayed dark adaptation.
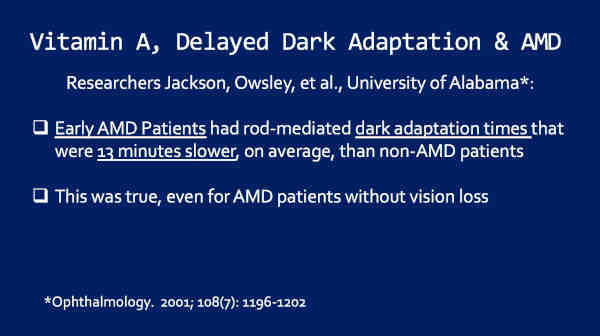
So these researchers, Jackson, Owsley, and colleagues, University of Alabama, found that early AMD patients had dark adaptation times that were 13 minutes slower, on average, than non-AMD patients.
Now, this is a strong suggestion that they’re vitamin A deficient.
This was true, even for AMD patients without vision loss.
So this is, again, a very strong indication that they’re vitamin A deficient. But, they took this a step further.
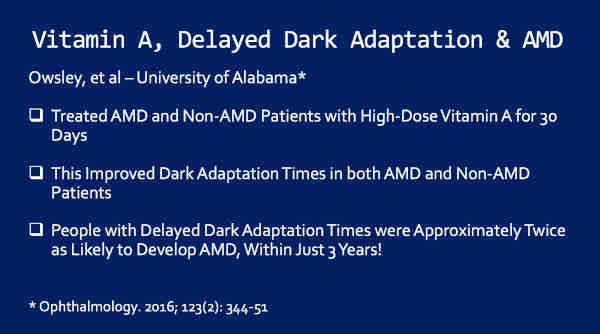
They treated both AMD and non-AMD patients with high-dose vitamin A, for 30 days.
And what they found was that this improved dark adaptation times, in both AMD and non-AMD patients.
So if the AMD patients had delayed dark adaptation times, that might mean they’re vitamin A deficient or they have a perturbed mechanism to get vitamin A there [to the retina proper].
But, if vitamin A improves the dark adaptation times, for both AMD and non-AMD patients, it means that they’re truly all vitamin A deficient! Even the non-AMD patients.
But this is a strong indication that vitamin A is a major factor here.
Now, this is the most important ‘take home.’ People with delayed dark adaptation times were approximately twice as likely to develop AMD, within just three years.
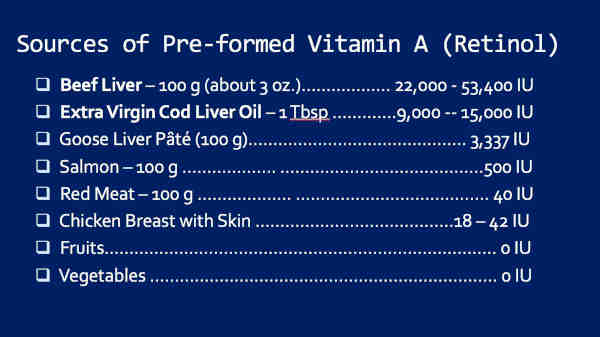
So, where do we get vitamin A? Here’s some possibilities:
Beef liver — fantastic source! Twenty-two thousand [22,000] to 53,000 IU’s in three ounces.
Extra virgin cod liver oil [EVCLO] — 9,000 to 15,000 IU’s per tablespoon.
Look at chicken breast with skin — 18 to 42 IU’s.
Fruits and vegetables — none! Right? You can get vitamin A from fruits and vegetables through carotenoids, but the conversion is highly inefficient. As little as one in thirty molecules may be converted. It’s based on genetics, microbiome — gut microbiome — many things.
Okay finally, let’s look at vitamin K2 and macular degeneration.
Price called this ‘Activator X.’ He knew vitamin — or what he called ‘Activator X’ — worked in synergy with vitamins A and D, to produce wide facial structure, broad dental arches, uhm — straight teeth, healthy bodies, healthy bones. He knew all that, right?
In 2007, Chris Masterjohn published his works showing that Price’s ‘Activator X’ is vitamin K2.
And now we know that vitamin K2 drives calcium into teeth and bones, where it needs to be, right?
K2 deficiency leads to soft tissue calcification — vascular calcification.
So, I have hypothesized that K2 deficiency may result in calcification of Bruch’s membrane, producing more of a relative barrier between the choriocapillaris and RPE. This may be a major factor in macular degeneration.
And then a combination of K2 deficiency and oxidized LDL could lead to choroidal occlusion, was what we see [sic] down here.
So this all fits neatly together.
So where do we get K2?
Pastured chicken eggs.
Cheese from pastured cattle grazing on green grass. Same reason for pastured butter.
Right? Ruminants consume green grass, they get K1 — in their gut, they ferment that — to K2 — ends up in their milk. We consume it as butter.
Natto. Japanese natto is also an excellent source.
Okay, last part and we’re going to wrap up.
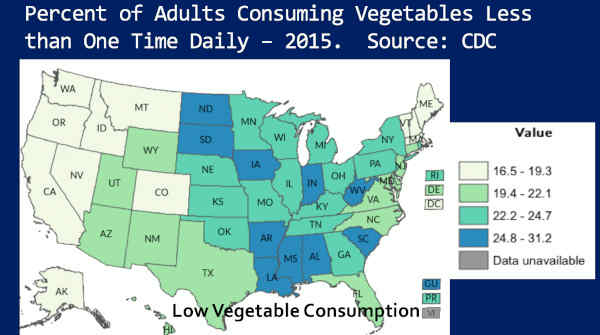
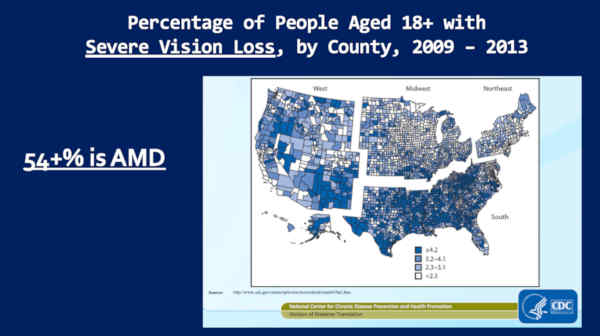
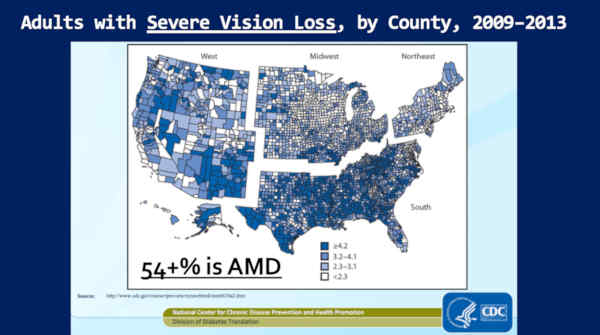
I think you’re going to like this. This is — these are ‘heat maps,’ I call them — from our own Centers for Disease Control [CDC].
This is the percent of adults consuming vegetables less than one time daily. So the darker colors are lower vegetable consumption. Alright? Light colors are higher vegetable consumption.
So I want you to notice that, right now, the low vegetable consumers in the South — high vegetable consumers in my home state of Colorado. I’m just going to use that as an example through this, okay?
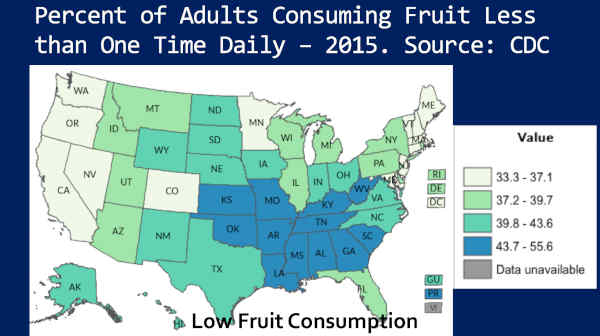
Next — percent of adults consuming fruit less than one time daily. Notice — low fruit consumers in the South — Colorado, high fruit consumers.
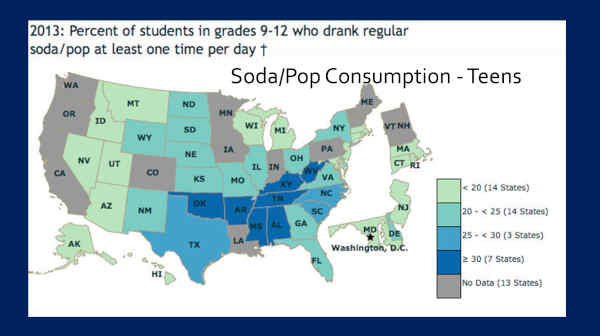
This, is soda pop consumption in teenagers. Notice — darker colors — higher soda pop consumption, in the South. Colorado had no data on this one.
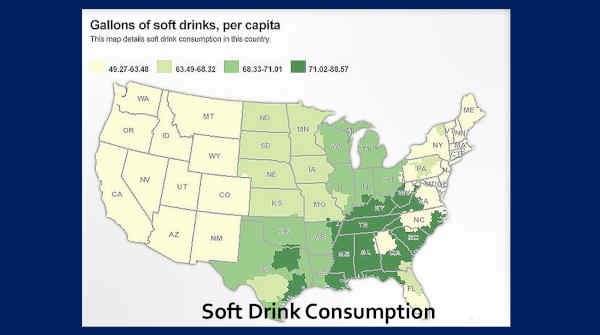
But, this is gallons of soft drink per capita — and the darker colors — higher consumption — notice it’s in the South. And notice that Colorado is among the lowest consumers of soft drinks.
So we pretty much already know where the processed foods are being consumed, right? Because nobody is living on meat, eggs, and dairy. Right? The only other thing left over would be wheat, if we’re not including these categories — or I mean, grains. And we know that most all of those in the U.S. are processed anyway — 85 percent.
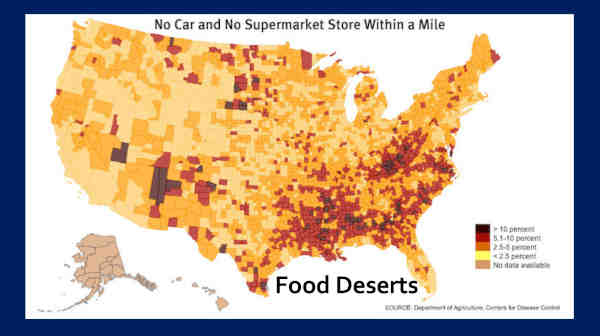
Okay, but the CDC takes this a step further. They looked at what they call ‘Food Deserts,’ which is defined as ‘No car and no supermarket store within a mile.’ Why is that important?
Because the CDC knows, if you don’t have a car and you don’t have a supermarket store within a mile, you’re consuming a lot of food from convenience stores.
And we all know, there’s no normal food — non-processed food — in convenience stores, right?
So now we know where the processed food is being consumed. And I want you to notice again, my home state of Colorado is low in ‘Food Deserts.’
Alright, let’s see what happens when we trace this.
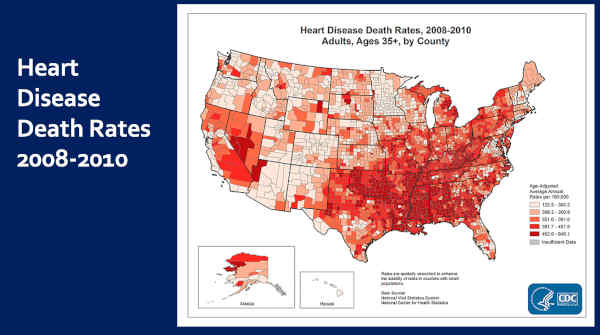
This is heart disease death rates, 2008 to 2010. This is where it’s worst, right? [pointing at map] In the South. Notice my home state of Colorado is where it’s lowest.
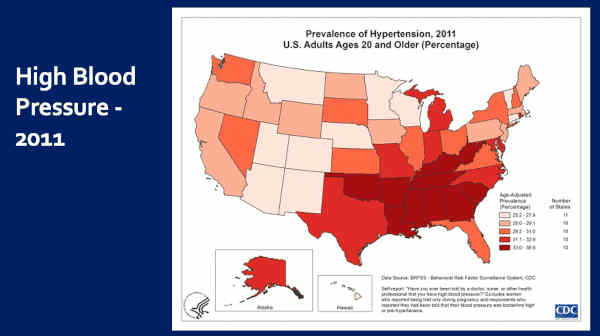
This is high blood pressure — 2011. Darker colors — worse — in the South. Notice, Colorado amongst the very best — the lowest prevalence.
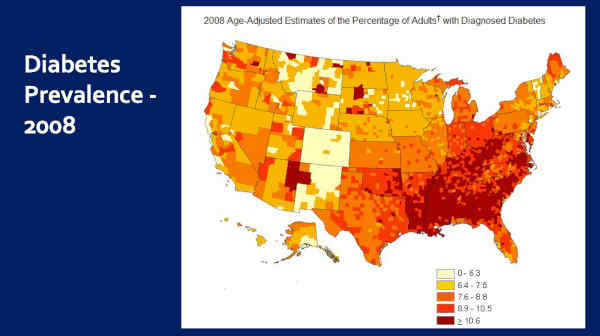
Diabetes prevalence — Worse in the South — Colorado among the very best.
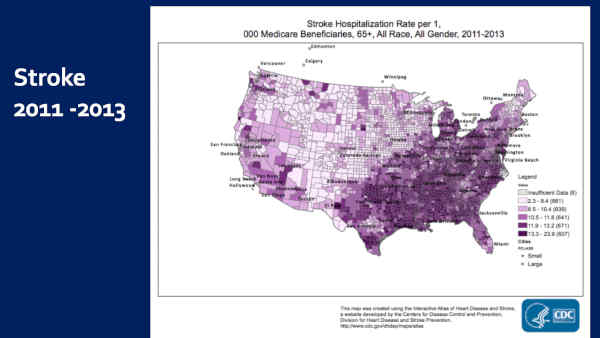
This is stroke. Worse in the South — Colorado amongst the best.
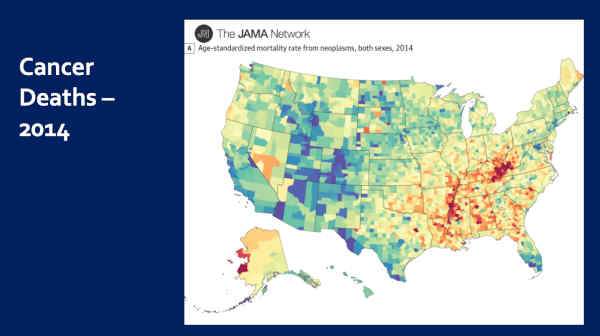
And this is cancer deaths. Now the dark reds and yellows — high cancer deaths. Blues and greens — low cancer deaths. Notice again, worse in the South, best in Colorado.
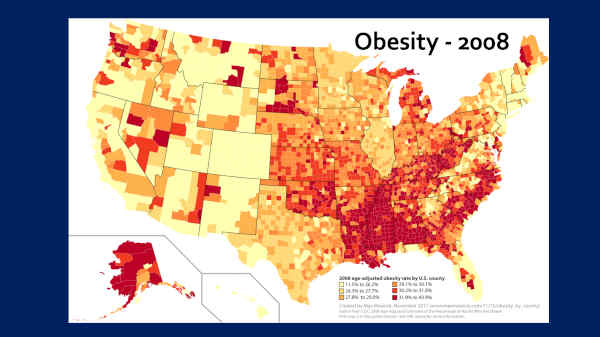
And this is obesity — 2008. You can see where it’s worst. And I want you to notice that Colorado has the lowest obesity in the nation.
So now we know where all the — we know where the processed food was being consumed — we know where all the Westernized disease is, right?
So I showed you all that, to bring you to this.
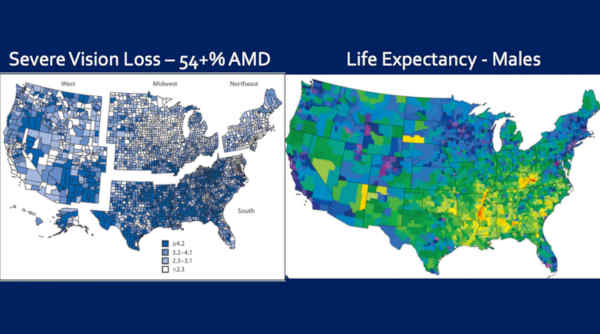
This is the percentage of people, aged 18 plus, with severe vision loss, by county.
Why is that important? Because, we’ve known that since 2,000, 54% of this severe vision loss is macular degeneration. It’s probably higher, because the last study ended in [year] 2,000.
So look where it’s worst. It’s the same map! It’s worse in the South — and Colorado, over here — is amongst the best.
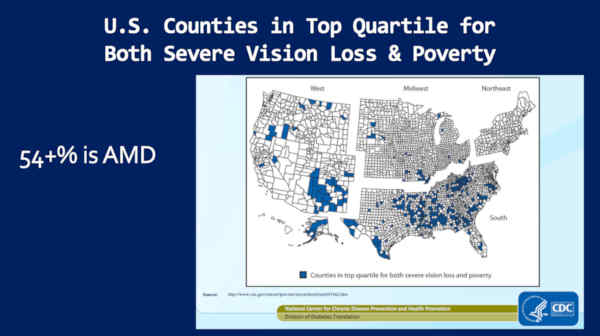
Now, I don’t like this next slide, but I’m going to show it anyway — because it’s reality.
This is U.S. counties in the top quartile for both severe vision loss and poverty.
And notice, it’s the — virtually — the same map. It’s the worst in the South and it’s the best in Colorado.
So why is it that poverty leads to blindness? Because that’s what we’re talking about here. Most of this vision loss is blindness — I mean, is due to — it’s not blindness — it’s due to macular degeneration.
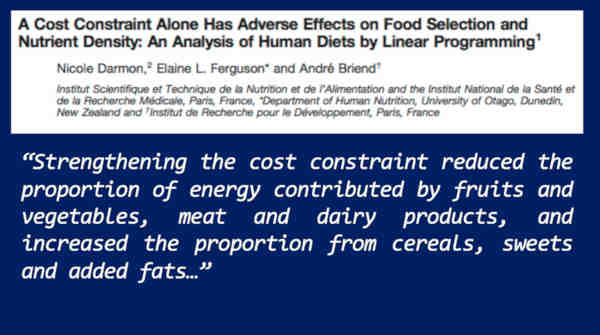
So, take a look at this study.
‘A Cost Constraint Alone — translated, budget — Has Adverse Effects on Food Selection and Nutrient Density.’ Now look at the quote.
‘Strengthening the cost constraint — again translated, budget — reduced the proportion of energy contributed by fruits and vegetables, meat and dairy, and increased the proportion from cereals, sweets, and added fats.’
Increased the proportion from processed foods, right?
And we know that the ‘added fats,’ 86% are vegetable oils.
This is why — the reason is — is that, in the U.S., you can buy 2,000 calories worth of processed food for about three-and-a-half dollars. You want that to be all non-processed food? It’s going to cost you at least 13 dollars, is what the research shows.
So let’s go back to this map.
Again, adults with severe vision loss.
Now, we know — again — most of this, this vision loss, is macular degeneration. Right?
But we’re told macular degeneration is a disease of aging, right? So if a lot of this — where all this macular degeneration is concentrated — these people should be living the longest, right?
Let’s see if that’s true.
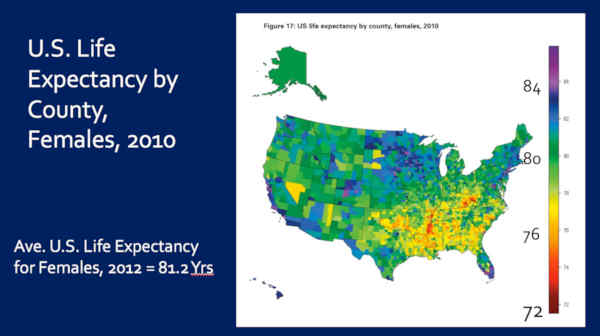
So here is U.S. Life Expectancy by County, for females, 2010. In the yellows, I’m sorry, in the reds — these are women living into their mid-70s, and yellows are about age 77 years. But notice the average U.S. life expectancy for females is 81 years at this time.
So the people with the most vision vision loss, have the shortest lives.
Let’s see if this is true for men.
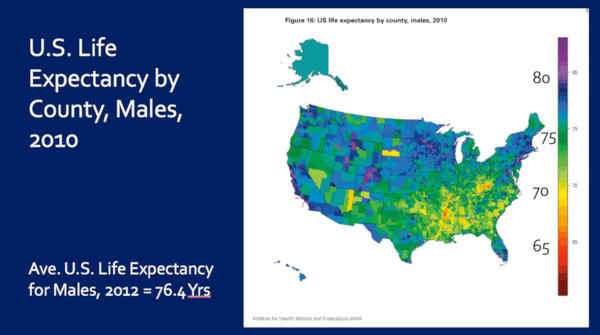
Here is U.S. Life Expectancy by County for Males. So, in the reds — these are men — there’s only a couple, but these are men living into their mid 60s, and in the yellows, they’re living to high 60s to 70-ish. But, the average U.S. life expectancy for men at this time — 76 years.
And if you notice my home state of Colorado, a lot of people — a lot of men — living into their 80’s. Right?
So this is Severe Vision Loss and Life Expectancy for Males, side-by-side.
And notice, again, that — you know — we’ve got the most vision loss down here in the South and the shortest lives in the South.
So, again, the bulk of this vision loss is macular degeneration — where people are living the shortest lives.
This is not consistent with the theory that AMD is a disease of aging. Right?
And if we’re to believe, that macular degeneration is a disease, driven by genetics, then are we also to believe that the same people, that consume the fewest fruits, the fewest vegetables, consume the most sugar-sweetened beverages, live in the most ‘food deserts,’ and therefore, have the most heart disease, the most hypertension, the most type 2 diabetes, the most stroke, the most cancer deaths, and the most obesity, just happen — by coincidence — to have the worst genetics for AMD?
(Audience laughter)
I mean, can you imagine — I think that is fantastically unlikely, don’t you?
Okay, one last slide, before we wrap up.
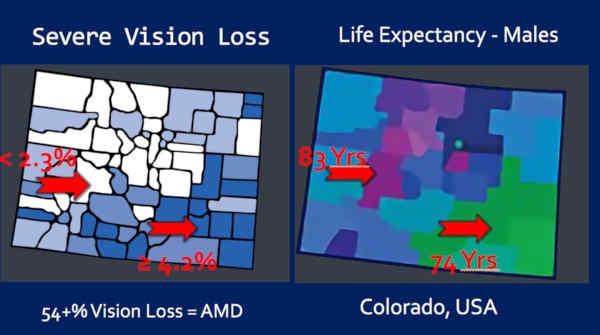
So this is my home-state of Colorado. You can do this with just about any state.
So take a look at the severe vision loss on the left — and life expectancy on the right.
In the white counties is where the severe vision loss is the lowest — less than 2.3%. Okay? The white counties. Notice that those are the same counties that — where the life expectancy is the longest — 83 years!
Now look at the counties in dark blue, where the — I’m sorry — the vision loss is the greatest — greater than 4.2% — about twice as much — twice as much macular degeneration, is where the men are living the shortest lives — 74 years. Nine years shorter, on average.
Ladies and gentlemen, macular degeneration is not a disease of aging or genetics, it’s a disease of processed food consumption.
(Applause)
Thank you, I’ll wrap up. Okay.
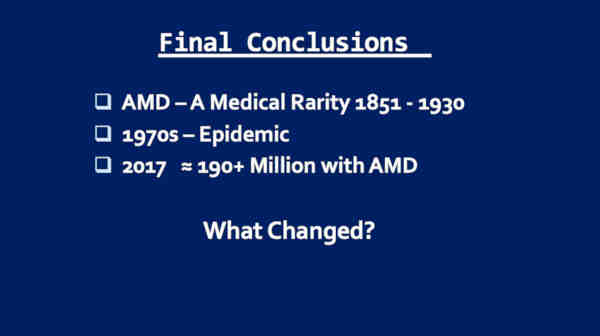
So, AMD was a medical rarity from 1851 to 1930. I don’t believe there’s any question about that.
By 1970s it was epidemic.
By 2017, over 190 million people, today, with AMD.
What changed?
Well, you know what changed. The ‘displacing foods of modern commerce,’ are what changed.
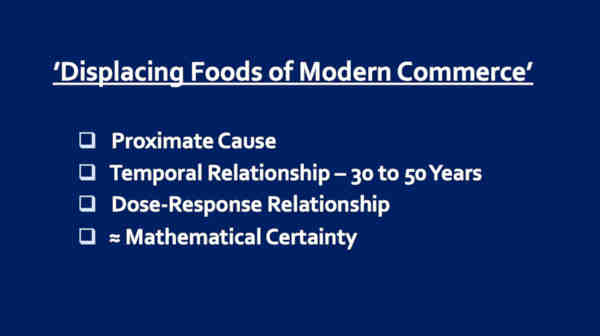
We have evidence for proximate cause, because if you look at all 25 nations, the processed foods always come first, then the AMD. It’s never the other way around.
The temporal relationship — at least 30 years of consumption.
There’s a dose-response relationship. You’ve seen it — 0.1% prevalence of AMD in the Africans of Southwestern rural Nigeria, who can’t get processed foods, versus AMD prevalence of 24.3% — or 243 times greater — in the Africans of Barbados, where the norm is processed food.
And finally, if you look at all 25 nations, I think you’ll all come to the same conclusion I did. This is nearly a mathematical certainty that this relationship exists.
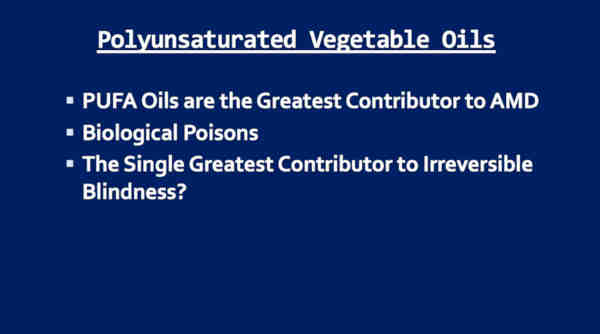
So, the PUFA vegetable oils deserve special mention. I love them, you know? Right?
I believe they’re the greatest contributor to AMD.
Biological poisons is what I call these.
They’re the single greatest contributor to irreversible blindness, I believe.
But the big picture is this — ‘Displacing Foods of Modern Commerce’ lead to AMD. That’s the take-home message.
This is not ‘Age-related Macular Degeneration,’ ladies and gentlemen.
This is Diet-Related Macular Degeneration.
We propose that the name of this disease be changed from AMD to DMD — Diet-related Macular Degeneration — so people will begin to focus (applause) — thank you — so people will focus on the true cause.
And so I’m asking you, if you believe this hypothesis has validity, to become acolytes of this — spread this message with me. I know you all will, and I thank you for that, because 190 million people are losing vision to this disease.
And this breaks my heart, but 270 people will go blind today. They’ll lose vision in their second eye, due to macular degeneration, today. They lost it in one, and today they’ll lose their second eye.
And this is tragic.
And I believe it is all preventable.
So our mission, at Cure AMD Foundation, is to prevent and treat macular degeneration through ancestral dietary strategy, advocacy, and more scientific research.
You know we can’t convince physicians and ophthalmologists based on what I presented to you today. It’s going to take more. We need to do more.
Our organization, Cure AMD Foundation, can be found at CureAMD.org. We have lots of free resources. I do have a book available there.
I want to thank Sally Fallon-Morell and I want to thank the Weston A. Price Foundation, and I want to thank all of you.
It has been an honor and a pleasure. Thank you.
(Applause)




















Recent Comments