by Chris A. Knobbe, MD
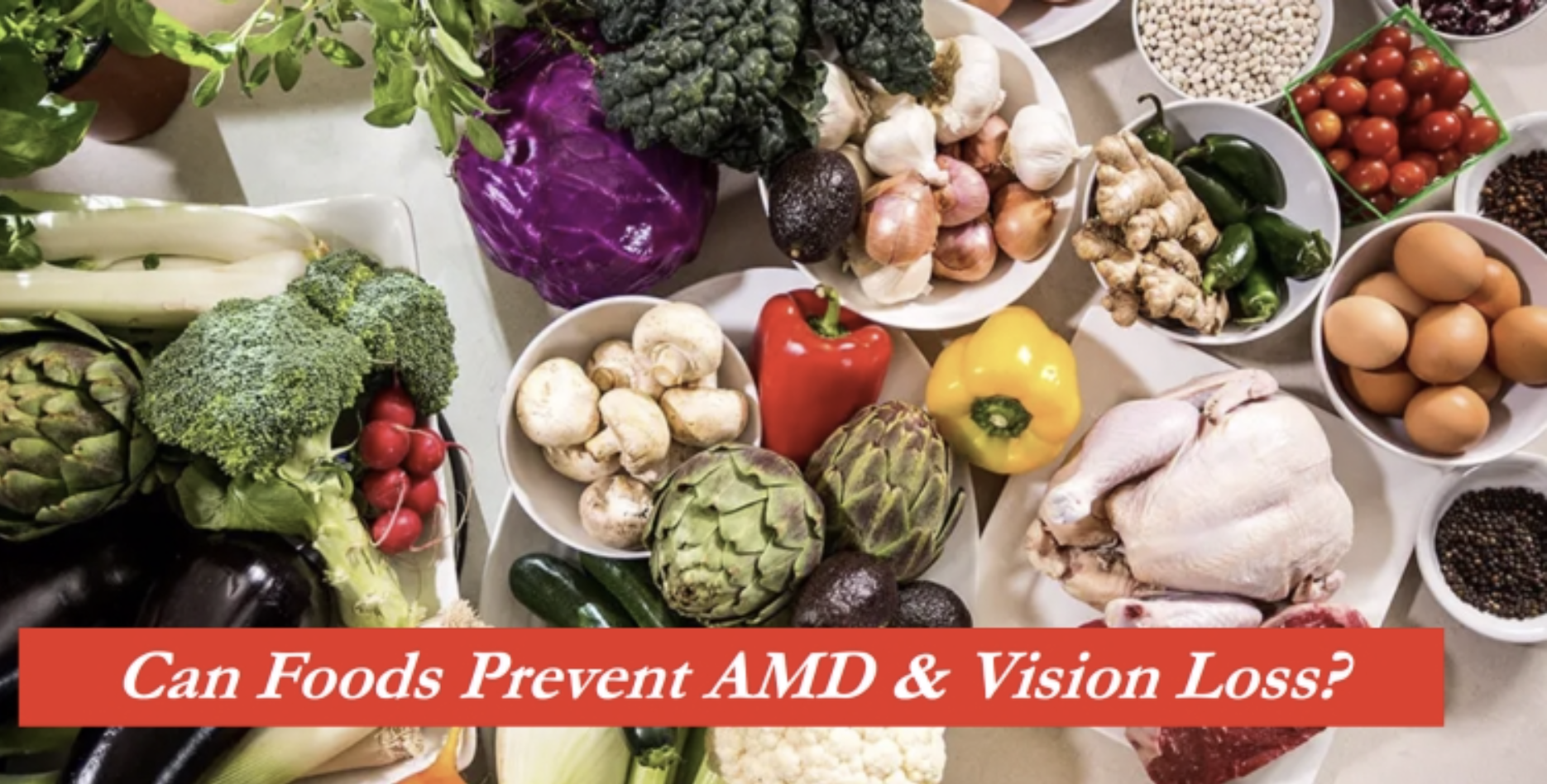
Perhaps the better title for this article might be, “Are the AREDS formula vitamins better than a ‘healthy’ diet?” Or alternatively, “Should vitamin supplements, such as the AREDS formulae, be the primary focus of treatment for dry age-related macular degeneration (AMD)?”
In the book that I authored on this subject, Ancestral Dietary Strategy to Prevent and Treat Macular Degeneration, I wrote a chapter on this subject, entitled, “Synthetic Vitamins and Multivitamins – Should We Steer Clear?”
In this article, I’ll review some of what I’ve written for the book chapter. I’ll expand in some areas – I’ll skip some areas for brevity – and in other areas I will bring to light subject matter that has arisen since I completed the research for the book, in early 2016. In both cases, the end-results and my recommendations will be the same.
Ladies and Gentlemen, this is an uber-long article. It has to be. No short review will ever do this subject justice. And just like the book that I’ve published on this subject, my goals are clear…
I intend to provide the background, history, fundamental science, and even the evidence-based research, that could literally save your vision.
That’s what is at stake here – your vision. And, of course, your pocketbook, since consuming vitamin supplements over the coming years could cost you thousands of dollars.
But, it’s your vision that is priceless, right?
To that end, let’s embark on this journey (through this article) together, because if you stay with me, through every step of the way, I believe you will find the conclusions quite literally, shocking. If you skip to the end for my recommendations, you’ve missed the point. You won’t “get it,” I assure you…
As we approach this subject, I think it is befitting for us to recall that around 400 B.C., the ‘Father of Medicine,’ Hippocrates, wrote, “Let food by thy medicine and medicine be thy food.” For those who are enlightened as to the benefits of ancestral nutrition, Hippocrates’ quote serves as a powerful reminder as to the power of food.
First, to Dispel the Myth of “Eye Vitamins”
Right off the bat, let’s get one thing straight. There’s no such thing as “eye vitamins.” Just like there is no such thing as “brain vitamins,” “liver vitamins,” “heart vitamins,” or any other organ specific vitamins.
There are 13 vitamins that are required by humans, and these must be supplied through consumption, or in the case of vitamin D, through exposure of our unprotected skin to sunshine.
These vitamins include the fat-soluble vitamins: A, D, E, and K and the water-soluble vitamins: B1 (Thiamine), B2 (Riboflavin), B3 (Niacin), B5 (Pantothenic acid), B6 (Pyridoxine), B7 (Biotin), B9 (Folate), B12 (Cyanocobalamin), and vitamin C.
Every single cell of every single organ and organ system, depends extraordinarily so on all of these vitamins, as well as minerals and other cofactors that are required for optimal function. Our scientific knowledge of these fantastically complex, synergistic relationships, between all of these vitamins, minerals, and other nutrients, still remains in its infancy.
But what I intend to show, in this article, is that certainly a number of vitamins (likely all 13 of them) are required, necessary, and beneficial in both preventing and treating macular degeneration, but these vitamins most optimally must be obtained from food. That’s correct. From food. Real, natural, whole, preferably organic foods and, in fact, some very particular foods that also supply the hard to come by fat-soluble vitamins, which are not widely distributed in the food supply.
 Yes, I intend to show that these vitamins and other nutrients should, most optimally, not come from pills, tablets, “fortified” foods, which are those with artificially placed synthetically derived vitamins, or any other supplements, including the AREDS formula vitamins (such as Bausch and Lomb PreserVision, PreserVision AREDS, MacularProtect AREDS2, ActiveEyes AREDS2, ICaps AREDS Formula, Ocuvite, Ocuvite with Lutein, Pro-Optic AREDS 2, Visionary AREDS-2, Macular Shield AREDS 2, etc., etc., etc.).
Yes, I intend to show that these vitamins and other nutrients should, most optimally, not come from pills, tablets, “fortified” foods, which are those with artificially placed synthetically derived vitamins, or any other supplements, including the AREDS formula vitamins (such as Bausch and Lomb PreserVision, PreserVision AREDS, MacularProtect AREDS2, ActiveEyes AREDS2, ICaps AREDS Formula, Ocuvite, Ocuvite with Lutein, Pro-Optic AREDS 2, Visionary AREDS-2, Macular Shield AREDS 2, etc., etc., etc.).
Even far more importantly, I intend to also discuss the hypothesis for the true cause of AMD in this article – which has everything to do with the issue currently at hand, i.e., vitamins and AMD. That hypothesis, to be revealed in this article, along with our supportive research, is pending publication in the peer-reviewed journal, Medical Hypotheses, at this time.
So, let’s begin, shall we?
A Little History on AMD…
Before we examine the benefits, faults, risks, and even the reduced lifespan of those consuming synthetic multi-vitamins (yes, it’s true, and AREDS formulae are multivitamins), it only makes sense to review just a glimpse of the medical history that I uncovered, when I dug deep into the scientific literature on the subject of macular degeneration. Why look at the history of macular degeneration, you may ask?
The answer lies in the fact that the history of the increasing incidence and prevalence of AMD and the history of the modern refining and Westernization of the diet, are deeply correlated. We’ll come back to this.
I’ll only briefly touch on the history of AMD here, because I’ve covered this in minor detail in the Introduction article located on this site, and in far greater detail in my book on this subject.
In brief, I completed an extensive review of the historical scientific literature on macular degeneration, and found an abundance of evidence that would lead us to believe that macular degeneration was an extraordinary medical rarity, from 1851 until about 1930.[1] Perhaps just as importantly, I couldn’t find even a shred of evidence, anywhere, in any scientific paper, textbook, or atlas, which might lead us to believe that macular degeneration was not rare during that period of time.
This historical medical literature search also supports the conclusion that the prevalence of AMD began to climb in the 1930s, in both the U.S. and the U.K., such that by the 1970s, at least in the U.S., macular degeneration had elevated to epidemic proportions.1 The U.K. followed suit – and many other developed nations were in the queue for epidemics of AMD at that time, with AMD prevalence rising to double digits by the 1990s and early 2000s for many nations.[2]
Here are just a few highlights from more than a century’s worth of literature…
- Herman von-Helmholtz invented the ophthalmoscope and published its design,
 in 1851.[3] This allowed ophthalmologists, for the first time, to begin to view the fundus (macula, optic nerve, vessels, and retina)
in 1851.[3] This allowed ophthalmologists, for the first time, to begin to view the fundus (macula, optic nerve, vessels, and retina)
Helmholtz’ ophthalmoscope design spread throughout the world, within a decade of his publication.(3) That is, ophthalmologists were using ophthalmoscopes all around the world, by 1861.
- By the mid 1850s through the 1870s, ophthalmologists were producing illustrations and atlases of the retina (including macula) of the eye, yet none of the images depicted macular degeneration.[4] Today, macular degeneration is the most commonly encountered retinal condition, affecting nearly one in three people over the age of 75.[5]
- In fact, twenty-three years would pass after Helmholtz’ invention, before
macular degeneration was described for the first time. Ophthalmologist, Jonathan Hutchinson, of London, England, presented four cases with descriptions consistent with macular degeneration, that he had collected in his practice. There were no pictures or illustrations of these cases, but the text descriptions were consistent with probable macular degeneration. The year was 1874. [6]
- In 1880, ophthalmologists Landolt and Snellen had collected 86 different types of ophthalmoscopes in use around the world.[7]
- In 1889, famed Austrian physician, ophthalmologist, and professor, Ernst Fuchs (1851 – 1930), published his Lehrbuch der Augenheilkunde (English translation, Textbook of Ophthalmology), of just under 800 pages in length. The book was translated into English in 1892. Though he dedicated some 40 pages of the book to conditions of the retina and choroid, he wrote only one sentence regarding macular degeneration: “Finally, a disease of the macula is observed in old people, which usually affects both eyes about equally, and is referable to senile changes.” [8]
- In 1889, Fuch’s Textbook of Ophthalmology reviewed that six different mydriatic (pupil dilating) agents were in use, including Atropine, Cocaine, Homatropine, duboisine (also called hyoscyamine), hyoscine, and gelsemine.[9] Obviously, ophthalmologists were dilating patient’s pupils, routinely, even by the 1860s and beyond.
- In 1895, German ophthalmologist Otto Haab, published a paper in which he had evaluated some 50,000 ophthalmic patient records, and concluded that macular degeneration was about as rare as myopic maculopathy and traumatic maculopathy, both of which are exceedingly rare conditions.[10] [11]
- On the occasion of the 50th anniversary of the ophthalmoscope, in 1901, an exhibition was put on in Atlantic City, New Jersey, where no less than 140 different brands and/or versions of ophthalmoscope were on display.7
- By 1913, ophthalmologist Edward Landolt reported that 200 different models of ophthalmoscope had been produced worldwide.7
- In 1920, the U.S. Census Bureau showed that there were 4.9 million people over the age of 65, as compared to 35 million over the age of 65 by year 2000. If the same prevalence of AMD existed in 1920, as it did in 1990 (22.8% of those aged 43 to 86 years),[12] there should have been over 1.1 million people affected with AMD in the year 1920. Yet, there were perhaps no more than 50 cases of AMD documented worldwide to that point.[13]
This latter point defeats any possible speculation that there wasn’t a high prevalence of AMD due to the absurd and ridiculous old canard that ‘people didn’t live as long.’ I’ll deal with this, in great detail, in an upcoming article, but the belief system that people ‘didn’t live as long,’ comes from math-challenged individuals who don’t understand the difference between longevity (which is the typical lifespan of an individual who does not die prematurely due to infections, accidents, war trauma, etc) and average lifespan.
- In 1927, the eminent and prolific ophthalmologist, Sir Stewart Duke-Elder, of Great Britain, published his first comprehensive textbook of ophthalmology, Recent Advances in Ophthalmology. The text was some 340 pages in length, yet missing from the entire textbook was any mention of macular degeneration. In fact, in the opening pages of the book, Duke-Elder wrote, “The two ‘major’ diseases of ophthalmology, cataract and glaucoma…” 14
Typical of most any ophthalmology textbook of that era, there was no mention whatsoever of the condition of macular degeneration.[14] Duke-Elder gave substantial attention to other retinal conditions, however, which had been the case in most textbooks of ophthalmology, since the 1850s and 1860s.
- In 1940, when Duke-Elder’s published his next textbook of ophthalmology, he dedicated some 13 pages to the condition of macular degeneration, including 17 images, six of which were in full color. In stark contrast to his 1927 text, he wrote, “Senile Macular Degeneration, first described as a clinical entity by Haab (1885), is a common cause of failure in central vision in old people.” [15]
- By 1966, Duke-Elder, in his textbook series, System of Ophthalmology, published in 1966, wrote, “SENILE MACULAR DEGENERATION, first described as a clinical entity by Otto Haab (1885), is a common cause of failure in central vision in old age, occurring in some 25% of people between 65 and 80, and 30 to 40% over the age of 80 years.” [16]
In my own exhaustive search regarding the history of AMD, I believe that Duke-Elder may have been the first ophthalmologist to recommend synthetic vitamins for AMD. In his 1966 textbook, he wrote, “Perhaps the most useful – and innocuous – method of therapy is an abundance of vitamins associated with nicotinic acid [vitamin B3, or Niacin].” 16
Duke-Elder’s assertion that the synthetic vitamins were “innocuous” will be challenged in this article. However, at the time that Duke-Elder made the statement (1966), there was no research to indicate the potential harm (and general lack of benefit) of synthetic supplements.
- By 1973 to 1975, the United States’ Framingham Study, in Framingham, Massachusetts, published findings that some 8.8% of subjects between the ages of 52 and 85 years had AMD, while 27.9% of those between the ages of 75 and 85 had the disease.[17] [18] [19]
This indicates an epidemic of macular degeneration, with over four million Americans affected.
Though I’ve just picked a few of the most salient and cogent pieces of historical medical evidence for this article, I hope you’re beginning to see, that in the court of medical evidence, macular degeneration was unquestionably a medical rarity until 1930. In fact, it appears that the disease was almost non-existent between 1851 and about 1930.
The evidence then strongly suggests that the disease began to increase in prevalence in the 1930s and, of course, rose to epidemic proportions by the 1970s, at least in the U.S. and U.K., as I wrote previously.
‘So, why is this important’ you ask?
Well, if AMD were once a medical rarity, especially just about 85 years ago and prior, then how can we…
- Consider this a disease of aging or genetics, and/or
- Believe that synthetic vitamins, or multivitamins, would be the most beneficial way to treat this disease?
With regard to aging and/or genetics as causes of AMD, neither could possibly explain the dramatically increased prevalence of AMD. I’ve dealt with this in great detail in my book, and briefly in the Introduction page of this site.
Given that this article is intended to deal with the question as to whether synthetic vitamins should play a role in the treatment of existing macular degeneration, which includes the AREDS (Age Related Eye Disease Study) vitamin formulae, I’ll deal with that question almost exclusively in this article.
Did Our 19th Century Ancestors “Take” Multivitamins?
Hopefully, the above question alone should lead us to believe that synthetic multivitamins would not be necessary, either to prevent or to treat, macular degeneration. Note: synthetic vitamins are not purported or believed by any authorities to prevent macular degeneration – only to treat macular degeneration. We’ll delve into that research, shortly.
And in case you’re wondering why I have been prefacing the term “multivitamin” with the term “synthetic,” it is because I want to make a clear distinction between vitamins that come in the form of pills and tablets, from those that come in actual food. After all, they behave in dramatically different ways, as you’re about to see.
So let’s examine the history of vitamins, just briefly. We need this perspective and context, in order to assess any potential benefits of consuming multivitamins for the management of AMD.
Bear with me, but I believe this history is absolutely critical to understand how and why we’re obsessed with and still somehow convinced that the consumption of synthetic vitamins will cure (or treat) many ills, including macular degeneration, when we’re constantly faced with failures in this regard. Alright, moving forward…
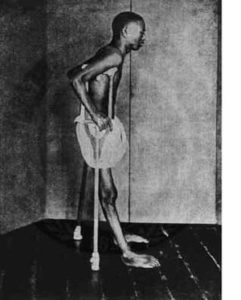
Biochemist Kazimierz Funk, whose name is commonly anglicized to Casimir Funk, is credited with formulating the concept of vitamins, in the year 1912.[20] Funk proposed the concept of these “vital amines” or “vitamines,” which was later shortened to “vitamins,” as he took part in research that attempted to discover the cause of the neurological condition, beriberi.
Beriberi, which is a dreaded condition of neuropathy, has both “wet” and “dry” forms. “Wet beriberi” is characterized by congestive heart failure with massive edema (swelling) of the legs, while “dry beriberi” is characterized by a peripheral neuropathy with severe pain and weakness in the legs, numbness, and extreme emaciation despite near complete appetite loss. The condition often led to death by suffocating convulsions. Between 1878 and the early 1900s, one thing gradually became clear regarding beriberi: the disease seemed to occur primarily in those consuming a monotonous diet, consisting mostly of polished white rice. Funk proposed that beriberi was the result of a deficiency of a “vitamine,” a term shortened from his original “vital amine.”
In this particular case, Funk believed the missing “vitamine” was a substance present in brown rice, but not in white rice – and he was right.
At that time, in fact, Funk described the now obscure conditions of beriberi, scurvy, rickets, and pellagra, all as ‘deficiency disorders,’ that is, that each condition was caused by the lack of a certain “vital-amine,” where ‘vita’ indicates ‘life,’ and ‘amine’ was equal to ‘a nitrogenous substance essential for life.’ 20
In 1933, Robert Runnels Williams (1886 – 1965), a dedicated chemist, finally isolated the nutrient missing in the diet of those afflicted with beriberi. That vitamin was thiamine, or vitamin B1.[21] This vitamin was eventually mass-produced and used to “fortify” foods to prevent beriberi.
Notably, beriberi was a disease caused by an extremely monotonous, bland diet, consisting largely of polished white rice. Interestingly, it was the polishing of the rice that led to the removal of the husk and, therefore, the removal of the B vitamins.
Similarly, scurvy was a disease primarily of sailors and could affect nearly half of any ship’s crew traveling from Europe to the Caribbean, due to the lack of vitamin C. This occurred in the face of many weeks or months at sea without any fresh fruit or vegetables. But it wasn’t until 1932 that vitamin C was first identified and isolated.[22]
Rickets, a condition characterized by weakening and bowing of the bones, is secondary to vitamin D deficiency. In 1824, D. Scheutte first prescribed cod-liver oil to treat rickets.[23] Scheutte, of course, had no idea exactly what nutrient was in the cod-liver oil that led to its beneficial effect on the disease, but he knew it worked. Cod-liver oil had already been used for centuries for its many health-promoting benefits. Interestingly, when the oil of fish liver is properly extracted and stored, it is a tremendous source of both vitamin D and vitamin A.
Despite the fact that Scheutte had properly treated and cured rickets with cod liver oil, it would be more than a century after his effective treatment, in 1931, before three different teams of researchers finally discovered vitamin D2, having isolated at least one of the active forms of vitamin D. One of those teams included German chemist, Adolf Windaus, who received the Nobel prize for chemistry in 1928 for his contributions to the understanding of sterols in relation to vitamins.23
Along the road to this discovery, however, the condition of rickets was determined by various researchers to be curable with certain components of an ancestral diet, including butterfat and cod-liver oil and, oddly enough, sunshine.23 Of course, we now understand that 7-dehydrocholesterol, a precursor to active vitamin D, is converted to vitamin D3 in the skin, when the skin is exposed to ultraviolet light.
Pellagra, a disease characterized by the “Four D’s,” which is photosensitive (sunlight induced) dermatitis,
diarrhea, dementia, and death, became endemic in the U.S. after 1902. Curiously, the disease primarily affected people in the Southern U.S. With thousands sick and dying, a physician by the name of Joseph Goldberger, MD, who was employed by the U.S. Public Health Service, was commissioned to discover the “infectious cause” of this disease. Goldberger had already shown great success in teasing out the cause of other infectious diseases, including yellow fever, dengue, typhus, hookworm, and diphtheria.
But what Goldberger found was that pellagra seemed to affect those consuming the typical diet of the Southern poor, which was meat, meal, and molasses. The meat was generally pork fatback, while the meal was cornmeal. This cheap, filling, monotonous diet, Goldberger was convinced, was missing a vitamin or vitamins, leading to the disease.
In 1915, Goldberger successfully treated those with the disease, by providing the affected with fresh vegetables, meats, milk, and eggs. This recovered those already affected, and prevented the disease in others.[24] But Goldberger’s discovery wasn’t accepted by the Southerners and, in fact, pride kept most from admitting that their diet might be at fault. Some even accused Goldberger of perpetrating a hoax.
So while Goldberger knew how to prevent – and successfully treat pellagra – with a healthy diet, the fact that he hadn’t isolated the missing nutrient prevented his theory and treatment from being accepted. Eleven years later, in 1926, Goldberger and his colleagues, on the basis of animal experiments, determined that the “pellagra preventive factor” was a water-soluble B vitamin. Goldberger died in 1929 and it wasn’t until 1937, that Conrad A. Elvehjem, a biochemist at the University of Wisconsin, finally isolated the nutrient, which was then called niacin, or vitamin B3.[25]
By the 1930s four major disease conditions, which had plagued, maimed, and killed hundreds of thousands of people, in some cases for centuries, were all found to be nutrient-deficiency diseases. Through most of history, the combined searches for the causes of these diseases remained highly elusive, primarily because physicians and scientists were in search of “germs” that were causative.
As Catherine Price, author of the book, Vitamania, so eloquently wrote, “Germ theory’s central tenet – that disease is caused by the presence of something—hid the idea that disease could also be caused by something that is lacking. Germ theory’s light was so bright, so illuminating, that it blinded scientists to the idea that disease could be caused by something that wasn’t there.” [26]
As it turned out, beriberi could be prevented and treated by the consumption of non-processed brown rice, rather than the processed, “polished,” rice. Scurvy could be prevented and treated with small amounts of fresh fruits or vegetables. Rickets could be prevented and treated with butter or cod-liver oil, or even sunshine. And finally, pellagra could be prevented and treated with a diet containing fresh vegetables, meats, eggs, and dairy.
Imagine, all of these diseases – preventable and treatable – with nothing other than healthy, well-rounded, whole-food based diets of both plant and animal origin? This should not be taken as a trivial, historical footnote.
The question is, will this have implications for macular degeneration?
So, back to the story…
Despite the fact that it was simply whole food that could both prevent and treat such diseases, the U.S. Government and many other nations’ governments who followed suit, didn’t promulgate to their people “healthy diets,” which could prevent such diseases. Instead, they began to “fortify” the very foods and diets that were causing such diseases, with artificially created or laboratory extracted vitamins, in bulk.[27] [28]
Fortification, the process of adding vitamins or minerals to a food, included the addition of vitamin D to milk in the late 1930s, “enrichment” of otherwise nutrient-deficient white bread made of refined white flour, with thiamine (B1) and niacin (B3) in the 1940s, ready to eat cereals (all of which are nutrient-deficient) made with added iron, B vitamins, and folate, and eventually, the addition of calcium to a variety of products beginning in the 1980s, just to name a few examples. 28 [29]
This truly has led to an odd paradox. The addition of synthetic vitamins to food—fortification or “enrichment”—has allowed us to consume the nutrient-deficient diets that have caused the nutrient-deficiency diseases in the first place.
As such, the Standard American Diet (SAD), as of 2009, is now made up of at least 63% refined, processed, nutrient-deficient foods in the form of refined white flour, refined and added sugars, polyunsaturated vegetable oils, and synthetically produced trans fats.[30]
This, in turn, has led to epidemics of “Westernized” diseases, such as heart disease, cancer, type 2 diabetes, Alzheimer’s disease, metabolic syndrome, hypertension (high blood pressure), obesity, and even autoimmune diseases, (I’ll reference all of this briefly) while the fortification has indeed prevented diseases such as beriberi, pellagra, scurvy, and rickets.
So the fascination with vitamins – in the form of pills – began. Despite failure after failure for such vitamins to achieve their intended benefits in literally thousands of studies in recent decades, our obsession with them continues. Even the medical orthodoxy has “taken” to this obsession.
Returning to our original question, clearly, our 19th century ancestors weren’t consuming synthetic vitamins. The concept of vitamins hadn’t even been conceived until 1912. Yet, only a few cases of macular degeneration existed anywhere on the planet.
Think about that…
“Westernized” Diets, Vitamin Deficiencies, and Degenerative Diseases
For those who haven’t read my book or the Introduction, it is worth reviewing here that, in 1939, Weston A. Price,

Weston A. Price Scientist, Researcher, and Dentist, often referred to as the “Isaac Newton of Nutrition.” 1870 – 1948
a highly accomplished scientist and nutrition researcher, published a treatise of nutritional and anthropological studies in his book, Nutrition and Physical Degeneration.[31]
During the period from approximately 1931 to 1937, Price scientifically and systematically studied populations on five continents, in fourteen nations, and among hundreds of different tribes and cultures and many thousands of people, he set out to determine exactly what diets led to excellent dental health versus dental decay, and good general physical health versus physical degeneration.
Price found, in virtually every single individual and population, that both dental health and general physical condition remained superb, as long as people consumed their native, traditional diets.
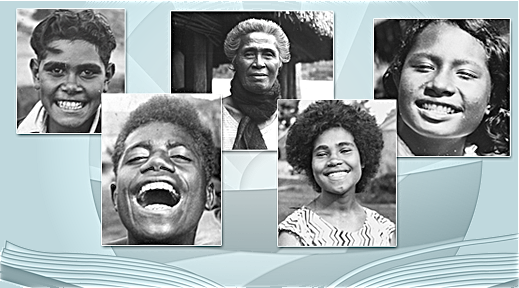
Typical facial structure and dentition of “primitive” people that Weston A. Price found to be consuming native, traditional foods. Image courtesy of the Price-Pottenger Nutrition Foundation (http://www.ppnf.org).
However, when people began to consume the foods that Price referred to as the ‘displacing foods of modern commerce,’ which he defined as consisting of refined white flour, sugar, canned goods, sweets, confectionary, and vegetable oils, they soon developed rampant dental decay, which was then followed by the onset of many degenerative conditions, such as arthritis and cancer.
Typical Dental Decay of People that Dr. Price Found to Have Transitioned to Westernized Diets. Image courtesy of the Price-Pottenger Nutrition Foundation (PPNF.org)
Another example of dental decay following transition to Westernized diet. Image courtesy of the Price-Pottenger Nutrition Foundation.
Young, growing children, consuming the processed food diets, developed facial deformities, with narrowing of the dental arches and consequently, misaligned teeth. Dental caries (cavities) often affected 20 to 30 percent or more of teeth in those consuming the ‘displacing foods,’ but generally around one percent or even less of those people consuming native, traditional diets.
Those consuming significant amounts of the ‘displacing foods’ were also far more prone to infectious diseases, which they once had immunity to, such as tuberculosis. Finally, Price found an onslaught of mental disorders in those consuming the processed foods, including suicidal ideation in those severely affected by dental disease, abscesses, and loss of teeth. Most of these societies had no dentists, nor any access to such, and the dental decay and abscesses meant chronic, severe, unrelenting pain and difficulty consuming the foods they once enjoyed.
Price analyzed the “primitive” people’s native, traditional diets, by sending thousands of food samples back to his labs in the United States. What he discovered was, by any analysis, shocking.
The “primitive” diets, which kept people brilliantly healthy, happy, and free of chronic Westernized diseases, contained at least ten times more fat-soluble vitamins (primarily A, D, and what Price referred to as the “X-factor, which is now believed to be K2), four times more water-soluble vitamins (all the B vitamins and C),[32] and approximately 1.5 to 60 times more minerals, than did the processed-food laden, Westernized (American) diets of his day.[33]
A boatload of more recent research is in support of Price’s principles. I’ll only mention some of the major research in this article…
Loren Cordain and colleagues, at Colorado State University, reviewed that the Industrial Revolution, with its attendant widespread production and consumption of refined vegetable oils, refined cereal grains (especially refined white wheat flour), and refined sugars, combined with the Modern Age “junk food” era, has resulted in numerous “maladaptive developments,” including numerous pathophysiological and degenerative diseases.[34]
Cordain’s group found that, currently in the U.S., pasteurized dairy, refined cereal grains (again, primarily refined white wheat flour), refined sugars, polyunsaturated vegetable oils, and alcohol account for some 70% of the total daily caloric consumption.[35] These five food groups are virtually entirely devoid of micronutrients, that is, vitamins and minerals.35
This is the recipe for metabolic disaster.
It’s worth repeating.
This is the recipe for metabolic disaster.
The above research, as completed first by Weston A. Price, and subsequently by Cordain and colleagues, as well as literally thousands of other researchers who’ve added to this body of work, draws correlative data between Westernized, processed food laden diets, and the numerous “diseases of civilization.” The latter, once again, include heart disease, numerous cancers, type 2 diabetes, metabolic syndrome, hypertension, Alzheimer’s disease, dementia, osteoporosis, gout, insulin resistance, obesity, acne, myopia (nearsightedness) and even autoimmune disorders, such as multiple sclerosis, rheumatoid arthritis, and many more.[36] [37]
All of the above mentioned diseases are either rare or virtually absent in hunter-gatherer populations and in those who continue their native, traditional diets.(37)
Westernized Diets and Macular Degeneration
Our own research draws the same correlations between increasing processed food consumption and increasing prevalence or incidence of age-related macular degeneration (see the Introduction for a brief review or my book, for full references and detail). We’ve analyzed this data in 25 nations – and the results are nothing short of compelling.
For those who don’t know the history of how our diets have gradually been overtaken by these nutrient-deficient, processed, man-made, and even toxic food components (e.g., sugars, polyunsaturated oils, and trans fats), please refer either to my Introduction, or book. Suffice it to say that the processed food elements have gradually replaced our own native, traditional, nutrient-dense foods – all of which primarily began – in 1880.
As the evidence clearly shows, the concept of vitamins wasn’t even officially promulgated, until 1912. We didn’t have any vitamins to supplement or fortify any foods, until the 1930s. Yet, this is the era – between 1851 and 1930 – when clearly, macular degeneration was a medical rarity. So does it make sense to subscribe to the tenet that synthetic vitamins are the most optimal way to treat this condition?
On a more personal note, virtually all of the nutrition researchers with whom I now most closely associate, have been educated by, espouse, and are aligned with the research findings and philosophy of Weston A. Price. This would include researchers such as Sally Fallon and the entire Weston A. Price Foundation team and scientific advisory board, the Price-Pottenger Nutrition Foundation scientific advisory board, Chris Masterjohn, PhD, Stephan Guyenet, PhD., Denise Minger, and many, many others.
In fact, all of the research that we’ve completed, which draws correlations between the incidence and prevalence of macular degeneration and processed food consumption in 25 nations, is founded upon the Weston A. Price principles.
Synthetic Vitamins – Will They Rescue Us From Macular Degeneration?
So, will the multivitamins rescue anyone from AMD? Will they prevent AMD? Halt its progression? Will they hurt
people? Even make macular degeneration worse? More complicated still, is the effect of vitamins on one’s AMD contingent upon their own genetics? These are a few of the questions that will be addressed, as we move forward.
Beginning right here, at this point in this particular text, is where almost all scientific papers, textbook chapters, and presentations begin on this subject. That is, the discussion usually begins with, “We assessed whether a multivitamin/multi-mineral supplement would prevent (or prevent progression) of age-related macular degeneration…”
There’s no background, no historical review of vitamins or synthetic supplements, no review or attention to the ever increasing consumption of nutrient-deficient, man-made, processed foods and all of the attendant chronic, degenerative conditions associated with such (e.g., heart disease, cancer, type 2 diabetes, obesity, etc.), little or no individual dietary history consideration, no historical view or review of the (increasing) prevalence of AMD throughout history, etc., etc., etc.
And the analysis I’ve given you thus far just begins to scratch the surface…
I’m not criticizing these researchers, or their studies. That’s exactly how we allopathic physicians, of which I am one, are trained. Anything that happened more than just a few years ago is immaterial. But this myopic approach leads to ever-increasingly absurd conclusions.
Less than a decade ago, my thinking process and viewpoint was the same as the typical allopathic physician. And that’s exactly where I thought the studies should begin. I’ve only been “enlightened” for about seven years (at the time of this writing).
And herein, I’m attempting to enlighten you as well.
Now, back to synthetic vitamins and AMD…
Let’s begin with a little background on studies that have assessed these issues, and I’ll do my best to be brief (it’s impossible, by the way, in order to do justice to this critical issue).
A Couple Studies Leading Up to the AREDS (Age-Related Eye Disease Study)…
The 1971 – 1972 National Health and Nutrition Examination Survey (NHANES), conducted by the U.S. Centers for
Disease Control (CDC), showed that diets rich in pro-vitamin A precursors (carotenoids), were inversely correlated to AMD development.[38]
The vitamin A precursors, generally known as the carotenoids (like beta-carotene, alpha-carotene, beta-cryptoxanthin, etc.), may be converted in the body to vitamin A, however, the process is inefficient, highly variable from person to person, and greatly dependent on a multitude of factors, including genetics, the gut microbiome (bacterial profiles in the gut), and the other foods consumed along with the carotenoids (e.g., saturated and monounsaturated fats increase absorption).[39]
And while we’re on the subject, the polyunsaturated “vegetable oils,” (I often place in quotes, because none of these are from vegetables, they’re seed oils primarily), have been shown to severely decrease the absorption of the carotenoids in the diet. These oils literally cause destruction of the carotenoids, unless significant antioxidants are present, which is often not the case.[40] For those not aware, our research has strongly implicated the polyunsaturated “vegetable oils” as major causative factors in AMD, with no less than ten studies in support.[41]
In 1994, Johanna Seddon, MD, Walter Willett, MD, and colleagues at the Massachusetts Eye and Ear Infirmary, published a landmark study in the Journal of the American Medical Association. That study showed that participants who consumed the most dark, leafy-green vegetables, like spinach and collard greens, had a 43% lower risk of developing AMD than did those who consumed the least.[42] Although this is one of the studies that actually addressed dietary elements, I point out this one because it likely influenced the AREDS 2 study, where lutein and zeaxanthin were given in the form of supplements.
So all of this began to lead investigators to the following question: Could synthetic vitamins, given in a pill, possibly prevent macular degeneration? So, let’s dig into this…
Do Synthetic Vitamins Prevent AMD?
For those unfamiliar with Cochrane, formerly known as the Cochrane Collaboration (the name many of us still prefer), it is an organization of around 37,000 scientists, researchers, and other professionals who work collaboratively as a global network to provide credible, unbiased health information. With that said, in 2012, Cochrane published their review which sought, “To examine the evidence as to whether or not taking antioxidant vitamin or mineral supplements prevents the development of AMD.” Their conclusion? They wrote, “We included four randomized controlled trials in this review; 62,520 people were included in the analyses. The trials were conducted in Australia, Finland and the USA and investigated vitamin E and beta-carotene supplements…. People who took these supplements were not at decreased (or increased) risk of developing AMD.” 43
Cochrane’s final conclusion reads as follows: “There is accumulating evidence that taking vitamin E or beta-carotene supplements will not prevent or delay the onset of AMD. There is no evidence with respect to other antioxidants supplements, such as vitamin C, lutein, zeaxanthin, or any of the commonly marketed multivitamin combinations.” [43]
In another recent review, published in the Annals of Internal Medicine, in November, 2017, the conclusion that antioxidant vitamins do not prevent AMD was, once again, confirmed by all available studies thus far, with that headline captioned below.
At least with all the available evidence in studies completed thus far, synthetic multivitamins do not appear to have any clear benefit in preventing the onset of AMD. So, if you think you might be able to stave off the development of AMD by taking your multivitamin, there’s not a shred of evidence to support that conclusion.
Moving on to the next logical question…
Do Synthetic Vitamins Slow Progression of AMD?
The next question is: Do multivitamin/multi-mineral supplements delay the progression of AMD, once it is already established? The Age Related Eye Disease Study (AREDS) sought to answer this question.
The AREDS trial, which lasted nearly six years before the first results were published, involved 3640 subjects, 55 to 80 years old, who were randomized to the AREDS supplement containing vitamins E and C, plus beta-carotene, zinc, and copper, versus placebo.
According to the AREDS researchers, for those with category 3 or 4 macular disease (category 3 is intermediate AMD and category 4 is advanced disease in one eye), “The risk reduction for those taking antioxidants plus zinc was 25%.“.[44]
However, this is relative risk reduction. What you want to know is your absolute risk, since relative risk is… well, relative.
Let me give you an example, where relative risk can make insignificant numbers sound massive. So, let’s say a research team wants to know if Drug A will help to prevent death from an ‘Ugly Disease.’ They give 100 patients the drug and 100 patients a placebo. One year later, 1 person died in the treatment group and 2 died in the placebo (control) group. The researchers then state this: “Drug A reduced the risk of death from ‘Ugly Disease’ by 50%.”
Why 50%? Because the relative difference in deaths is 1 versus 2, (1/2 = 50%). The research team proclaims a fantastic victory with a magnanimous drug that cuts the risk of death from ‘Ugly Disease’ by 50%!
But the absolute difference in deaths is just one person per 100 in the treated group versus 2 people per 100 in the control group, for an absolute difference of 1%. So now you know what your risk of death with treatment, or without (if you have ‘Ugly Disease’) – and that difference in this study was 1%.
Or might the difference just be due to chance? That’s where larger treatment numbers come into play and which allows us to calculate “statistical significance,” i.e., an attempt to statistically determine if the numbers are due to chance alone. We won’t go into that right now.
So, back to the AREDS…
For those with category 3 or 4 macular disease, at 5 years from the onset of the study, the probability of progression to advanced AMD was 28% for those given placebo, 23% for those given antioxidants (vitamins E, C, and beta-carotene), 22% for those given zinc, and 20% for those given antioxidants and zinc (the AREDS formula).44
From this, the difference between 20% and 28%, is just 8%. Eight percent is the absolute difference in numbers of patients progressing from intermediate AMD (or advanced AMD in one eye) to advanced AMD, during the five year follow-up. Eight percent of patients translates to 1 in 12.5, but since you cannot have half a person, this is one in 13.
That is, one in 13 was better, as a result of the AREDS formula.
And from this we get the Number Needed to Treat (NNT), which is also 13. That is, you will need to treat 13 patients with the AREDS formula, for one patient to benefit. Right, one out of 13 achieves a benefit.
I would like to mention a couple of additional findings that the AREDS investigators mentioned. In their own verbiage, “After accounting for age, sex, and race, participants in AREDS had higher or similar dietary intake of vitamins A, C, and E, and zinc than the general population sample from the Third National Health and Nutrition Survey (data not shown).” 44 This would indicate that the group was representative of typical Americans, at least in this regard, and this is exactly what we would expect, given that the study was completed at eleven centers around the United States.
Second, the AREDS investigators found that “Fifty-seven percent of AREDS participants were using a multivitamin or at least 1 ingredient found in the AREDS formulation at the time of their AREDS screening examination. About half of those supplementing were taking RDA doses rather than the 5- to about 15-fold higher doses of the AREDS ingredients.” 44
The investigators allowed the participants to continue their supplements. In fact, they provided Centrum without lutein, which is a widely available multivitamin/multimineral supplement with RDA level doses. They found that “Approximately 67% chose to take Centrum” 44 and a total of 13% of the AREDS participants who were not taking supplements before the study, then decided to also take a multivitamin “along with the study medication.” 44 This indicates that about 70% of the participants were taking a multivitamin supplement, whether they were in the actual treatment group, or the placebo group.
The point of all of this review regarding the additional supplementation is that, even in the placebo group, around 70% of them were receiving a multivitamin, which was typically Centrum. And all groups did very poorly, in terms of progression. Remember that 28% of those who had category 3 or 4 AMD to begin with, progressed to advanced AMD in 5 years, and that number was still 20%, even in the AREDS formula group.
The AREDS 2 trial, published in 2013, sought to determine whether adding the carotenoids found in dark leafy green vegetables, lutein and zeaxanthin, long-chain omega-3 fatty acids (docosahexaenoic acid {DHA} or eicosapentaenoic acid {EPA}), or both might further reduce the risk of progression of AMD.45
The conclusion from the AREDS 2 study: “Addition of lutein + zeaxanthin, DHA + EPA, or both to the AREDS formulation in primary analyses did not further reduce risk of progression to advanced AMD. However, because of potential increased incidence of lung cancer in former smokers, lutein + zeaxanthin could be an appropriate carotenoid substitute in the AREDS formulation.” [45]
In 2012, the Cochrane collaborative team evaluated all of the studies intended to evaluate the potential for antioxidant vitamins and minerals to prevent progression of AMD. They evaluated 13 randomized, controlled trials, which included a sum total of 6150 participants, including five trials in the USA, two in the UK, two in Austria, and one each in Australia, China, Italy, and Switzerland.
Cochrane’s final analysis: “The review of trials found that supplementation with antioxidants and zinc may be of modest benefit in people with AMD. This was mainly seen in one large trial [AREDS] that followed up participants for an average of six years. The other smaller trials with shorter follow-up do not provide evidence of any benefit.” [46] They added, “Although generally regarded as safe, vitamin supplements may have harmful effects.” (46)
By 2012, the evidence for the benefit of synthetic vitamins, in terms of preventing progression of AMD, wasn’t all that great. Out of the 13 trials that had attempted to address the hypothesis that antioxidant vitamins and minerals might help prevent progression of AMD, primarily only one showed any benefit – and that was the AREDS (1) trial.
No doubt, the AREDS trial was by far the largest trial and the longest lasting. In that trial, essentially one of thirteen patients had a benefit in terms of preventing progression. This benefit only occurred in those with at least intermediate degrees of AMD or advanced AMD in one eye. Interestingly, the greater the degree of AMD at the beginning of the trial, the more likely they were to benefit from the antioxidants and zinc.
** I would like to thank colleague Ophthalmologist and Vitreo-Retinal Surgeon, Andrew J. Luff, MA, MB, BS, FRCS, FRCOphth, of the United Kingdom, for his assistance in the AREDS analysis and statistics, in the sub-category above, entitled “Do Synthetic Vitamins Slow the Progression of AMD.”
AREDS Supplements Don’t Prevent AMD, But Are Expected to Prevent Progression of Disease – Is this a Paradox?
I’ve addressed this issue in my book – and would like to mention it again here. AREDS vitamins, or multivitamin antioxidant and mineral supplements, have not been shown to prevent AMD in any study.
Yet, we expect them to help prevent progression of AMD, once the disease is moderate or severe? Is this logical? Or is this a paradox?
If these supplements cannot prevent the disease in the first place, why should we expect them to prevent progression, once the disease is established?
Put on your logician’s hat, and think on that, if you would, and I’ll give my impression in the “Conclusion” of this article.
Synthetic Multi-Vitamin Supplements Cause Earlier Demise – and AREDS Formula is a Multivitamin
Wait, but the sub-title above is just an attention grabber, right?
Wrong. The sub-title above is true – and unequivocally so.
In 2012, the Cochrane (independent) researchers analyzed 78 trials that involved a total of 296,707 participants who were randomized to either antioxidant supplements, which included vitamins A, C, and E, beta-carotene, and selenium, or placebo, or no intervention at all (not even placebo). Fifty-six of these trials had a “low risk of bias,” (e.g., those that were not funded by vitamin manufacturers) and included 244,056 participants. The investigators found that those people taking the multivitamin supplements were 1.04 times as likely to die as were the controls.[47]
In other words, the people consuming the synthetic multivitamins were a little less healthy and likely to die a little sooner than those people not consuming synthetic multivitamins.
The Cochrane investigators wrote, in conclusion, “We found no evidence to support antioxidant supplements for primary or secondary prevention. Beta-carotene and vitamin E seem to increase mortality, and so may higher doses of vitamin A. Antioxidant supplements need to be considered as medicinal products and should undergo sufficient evaluation before marketing.” (47)
Oh, but you might be thinking, “Well sure, but that’s just one study, right?” Nah, this is a meta-analysis of 78 trials. Seventy-eight. And it was completed by Cochrane – an entirely independent organization, with no bias, whose only intent is to provide scientifically-minded advice for our benefit.
In a small cross-sectional study in Australia, 100 patients with Grade 3 or 4 AMD, who would ostensibly benefit from the AREDS formula (according to the AREDS Study), were interviewed to determine their knowledge and “compliance” with the regular consumption of the AREDS formula. Turns out that 53 percent of the participants were aware of the supplement, 38% were taking the supplement, and only 1% were taking the recommended dose (99% taking a smaller dose than recommended).[48] Among the 53% who were aware of the supplement, but not taking it, 31% cited cost as the main reason for not consuming the multivitamin. Another 31% were not taking the supplement either because of “actual side effects experienced, fear of potential side-effect and/or fear of interaction with other medications.” 48
This means that just about two-thirds of people not taking the supplement were doing so either because they were too expensive, they had already had side effects, or they feared potential side effects or interactions with other medicines. This means a good percentage of people are beginning to recognize the inherent potential side-effects and potential dangers of supplements – and this was a study published in 2006.
In another small study completed by investigators at Penn State University, in Hershey, Pennsylvania, researchers interviewed 64 patients with AMD, of whom 63% met AREDS criteria for vitamin supplementation. Of those who met the criteria for the vitamin supplements, only 43% reported taking the AREDS vitamins in the recommended dosages.[49] Interestingly, in this very small study, 75% of patients reported that “vitamin supplementation had never been recommended to them.” 49
The latter statement might possibly suggest that ophthalmologists and/or optometrists are not convincingly recommending the synthetic vitamin supplements to their AMD patients. Could this be?
As an anecdote from my own observations, I recall that, in December of 2014, when I was deep in the midst of investigating the hypothesis proffered herein (for the cause of AMD), I sat in a symposium for ophthalmologists at the University of Texas Southwestern Medical Center, among perhaps a couple hundred ophthalmologists. Ron Klein, MD, who is perhaps the U.S. expert on the epidemiology (incidence and prevalence of disease) of AMD, had just spoken and he was answering questions.
One ophthalmologist very directly asked Dr. Klein, “What do you really think of these AREDS formula supplements? Are they just snake oil?”
And perhaps the most interesting thing to me wasn’t his question (or the answer) really, but rather, the audience response. Nobody in the audience made a peep. No one sighed, gestured, shook their head, or in any other way appeared to react as if his question wasn’t appropriate. I was taking full notice, because I was about to begin a full-blown, full-time investigation into the cause of AMD that would forever change my life – and I had already began to develop the previously mentioned hypothesis and analyze the nutritional basis of AMD.
And, in fact, I was already deeply convinced that antioxidant vitamins bore little – if any – benefit for AMD patients.
Quite frankly, I don’t think a soul in that room had ever witnessed an exceptionally good response to the AREDS formula vitamins, but of course, this is pure speculation and conjecture on my part. I know that, in 24 years of ophthalmology, I never once saw a good reaction to the vitamin supplements. And quite honestly, I’ve never heard another ophthalmologist who has either.
Dr. Klein, of course, answered the doctor’s question, and with the usual… “Well, the AREDS formula did show that there was a 25% reduction… ” etc., etc.
Though I could fill the next five pages with reports on studies that have shown that synthetic supplements generally not only fail to provide their intended effects, but that they also may have significant side effects, let me just mention the ones most appropriate to the AREDS study.
In the AREDS1 trial, 7.5% of patients consuming the synthetic supplement had an increased risk of hospital admission for bladder and kidney complications from the high doses of zinc.(44)
In the AREDS 2 trial, there were more than twice as many lung cancer cases in those receiving beta-carotene (23 patients) as in those who did not receive beta-carotene (11 patients). That is, in smokers and former smokers, 2% of those receiving beta-carotene developed lung cancer, versus just 0.9% of those not receiving beta-carotene, and this number was statistically significant (P = 0.04).[50]
In a meta-analyses completed by investigators at Johns Hopkins School of Medicine regarding vitamin E supplementation and all-cause mortality, a total of 19 trials were evaluated to determine the overall effect. These 19 trials included a total of 135,967 participants; nine trials tested vitamin E alone and the other 10 tested vitamin E in combination with other vitamins or minerals. Their findings? In the authors’ words, “In our meta-analysis, we identified a dose-dependent relationship between vitamin E supplementation and all-cause mortality. Specifically, all-cause mortality progressively increased for dosages approximately greater than 150 IU/d [International Units/Day].” [51] And in their conclusion, they specifically state, “High-dosage (≥ 400 IU/d) vitamin E supplements may increase all-cause mortality and should be avoided.” (51)
Perhaps I should remind you (and me), the AREDS formula, including the AREDS 2 Formula, contains 400 IU of vitamin E!
Although I am still trying to keep my promise to keep this related to the AREDS formula, I feel compelled to mention – for those who really want to know about synthetic vitamin consumption, health and disease, just a couple things…
In a paper published in the journal Lancet, the authors open the paper with the following statement: “In observational studies, antioxidant vitamins [consumed in food] have been inversely associated with cardiovascular disease, cancer, and all-cause mortality. However, well conducted randomized controlled trials have shown that supplementation with antioxidants does not protect against these disorders (italics added).” [52]
For those still not convinced in the general lack of merit for such antioxidant vitamins in supplement form, I suggest watching two lectures, available online.
One of these lectures is by Howard Sesso, ScD, MPH, at the Harvard School of Public Health, entitled “Demystifying Nutrition – The Value of Food, Vitamins and Supplements.” [53] This is a Longwood Seminar, held at Harvard Medical School, and reviews numerous studies on synthetic vitamins and other supplements. It is available on YouTube.
The second is a lecture by Jeffrey Tice, MD, at the University of California San Francisco, Department of Medicine. This lecture is entitled “Vitamins and Supplements: An Evidence-Based Approach.” [54] This lecture is also available on YouTube and links for both lectures are available in the referenced footnotes (end of this article).
If you’ve generally been a fan of supplements, I think all of this may change your tune. And if it doesn’t, ask yourself if your current paradigm (and regimen) are properly benefitting you.
Alright, we’re making good progress. But, we’ve got a ways to go. The goal here is to leave no stone unturned. We want to know, for certain, that we’re doing the right thing, correct? How valuable is our vision? Is it not worth an intense investigation? I believe so. And I’m in this for you and your family, for me and my family, and for the more than 190 million other people in this world that are currently losing vision to AMD.
So let’s keep digging…
Macular Degeneration, AREDS Vitamins, and Genetics
So far, the findings have been pretty straightforward, right? With regard to macular degeneration, synthetically
derived vitamins (those in pills) don’t prevent AMD. But, they appear to help prevent progression of disease for those who have moderate or advanced AMD in at least one eye, and overall, about one in thirteen patients has a benefit. Not too good, but better than nothing most would agree, right?
But now the plot really thickens, the complexity elevates significantly, and the controversy begins…
Any researcher, science writer, or physician, who wants to teach, needs to try to take complex science or medical literature and make sense of it to those not in the field, right? Hopefully, I’ll do that as we deal with some complex genetics and AMD…
I will absolutely not exhaustively review the genetics versus vitamins and AMD research. I think it would overwhelm most anyone, including ophthalmologists and optometrists (unless they’re just gluttons for punishment!). So, I will just try to summarize the most salient research, in order to make sense of the big picture.
AREDS Vitamins Make Some Patients Worse, and Others Better?
In 2013, a paper was published in the journal Ophthalmology, by Carl Awh, MD, and colleagues, from the group, Tennessee Retina, located in Nashville, Tennessee. In this research, the authors analyzed the data from the AREDS trial, by correlating genetic make-up to AMD progression or stability, based on consumption of certain components of the AREDS formula. In short, the authors found that certain components of the AREDS formula may either be beneficial or harmful, depending on a patient’s genotype in the CFH and ARMS2 genes.[55]
CFH is the acronym for Complement Factor H and ARMS2 is the acronym for Age-Related Maculopathy Susceptibility 2 gene. Both of these genes are known to play a role in the genetic susceptibility to AMD. A certain polymorphism (variant) of the CFH gene, known as CFH Y402H, is associated with an increased susceptibility to AMD and this has been confirmed in multiple populations and multiple studies.[56] [57] [58] [59] [60]
Genetic variants at the ARMS2 genetic location, appear to increase susceptibility to AMD, in general.[61] The ARMS2 genetic variant, known as A69S, is a relatively strong risk factor for AMD.[62]
However, let’s keep the risk of these two genetic variants, in perspective. Because, even in the worst-case scenario, the increased risk is not as severe as one might think. Genes are carried as alleles, which means one from each parent; we can either have none, one, or two alleles (genes) of each type. If one has two copies of the CFH Y402H allele, they would develop wet AMD 2.8 years sooner, on average, compared to those who have no copies of the gene.[63] For those who have two copies of the ARMS2 A69S gene, they develop wet AMD 5.2 years sooner than an individual with no copies of the gene, again, on average.63
So, it’s not as if, let’s say you have the worst case scenario, genetically, that you’re going to get AMD 20 years sooner – that’s just not at all the case.
Alright, so back to the genetic make-up of an individual and their risk of AMD progression, based on AREDS supplements consumption.
In 2013, Carl Awh, MD, and colleagues, retrospectively analyzed 995 patients from the AREDS trial, who had category 3 (intermediate disease) AMD. They analyzed the outcomes of these patients, based on the genetic make-up of the CFH and ARMS2 alleles for each individual, stratified by whether the patients received antioxidants, zinc, both, or neither. They reported that patients with certain genetic profiles experienced more favorable outcomes with certain nutritional supplements, as compared to others.
In fact, Awh’s team reported that 49 percent of the subjects who received the AREDS formula were worse off than if they had received any of the other supplements. They also reported that, 13% of the group – those with high CFH and low ARMS2 risk genes, would have a more than doubling of progression of disease, if taking the AREDS supplement with zinc.[64]
In response to Awh’s research, the AREDS investigators then completed their own analysis of a subgroup of patients from the AREDS trial, for which they had genetic analyses. These 1,237 patients had either category 3 or 4 (intermediate or advanced) AMD. In this analysis, the AREDS investigators determined that there were no significant associations between genetic types and nutritional supplementation, stating, “At this stage, genetic testing does not appear helpful in improving treatment with AREDS supplements.” [65]
In 2015, Awh and colleagues then published yet another paper, analyzing some 989 patients from the AREDS trial, in patients with either category 3 or 4 AMD. Once again, they reported rather complex relationships between genetic categories, stratified based on the CFH and ARMS2 genes, and the various combinations of supplements. They indicated that, in their analysis, “most” patients would benefit from either no supplementation at all or a supplement other than the AREDS formulation, which included antioxidants and zinc.[66] By a “supplement other than the AREDS formulation,” the authors were referring to either antioxidants alone, zinc alone, or neither, given that the AREDS formula consisted of antioxidants (vitamins E and C and beta-carotene) plus zinc.
Awh’s group also argued that Dr. Chew and colleagues (who represent the AREDS study group), in dividing the study group into 27 different categories, induced a “lack of statistical power,” which resulted in data that failed “to demonstrate the benefit of the AREDS formulation for patients in any of the 27 subgroups.” (66)
If I do say so myself, I believe that Awh’s argument makes statistical sense, as some of the groups in the AREDS re-analysis had less than ten people. Out of the entire group of subjects, only 2317 had a genetic specimen, and only 882 progressed from no AMD, early or intermediate AMD, to advanced disease during the course of the trial. Each time this total number is reduced, by splitting into various categories, the statistical power of the study is markedly reduced.
In any case, in response to this second study by Awh and colleagues, the AREDS investigators, once again, attempted to replicate the analysis that Awh’s group had completed. In fact, the AREDS group identified 526 patients from the original trial, analyzed their genetics and outcomes based on the various supplement combinations, and reported that the findings by Awh et al could not be replicated. They reported that the original AREDS formulation, which consists of the antioxidants plus zinc, was the most beneficial nutritional supplement for all genetic groups analyzed.[67] The AREDS investigators advised against routine genetic testing, once again.
The American Academy of Ophthalmology weighed-in on this issue of genetic testing for AMD, in 2014, and they haven’t changed their stance since. The bottom line? They wrote, “Avoid routine genetic testing for genetically complex disorders like age-related macular degeneration…” [68]
In 2016, ophthalmologist Stephen G. Schwartz, MD, and colleagues, at Bascom Palmer Eye Institute, University of Miami, reviewed all of the evidence and in a paper published in the journal, Clinical Ophthalmology, they wrote “…at present there is not convincing evidence that genetic testing is beneficial in the routine clinical care of patients with AMD.” [69]
In 2016, professor of ophthalmology, Johanna M. Seddon, MD, and colleagues, of Tufts University School of Medicine, completed yet another analysis of the AREDS data with respect to the AREDS supplement groups. The conclusion segment of the abstract of their paper reads, very succinctly and simply, “The effectiveness of antioxidant and zinc supplementation appears to differ by genotype. Further study is needed to determine the biological basis for this interaction.” [70]
To say that there is disagreement on the issue is, obviously, quite an understatement.
Do We Give Awh’s Research the Benefit of the Doubt? Do We Genetically Test, & Then Choose a Supplement?
So maybe you’re just not convinced one way or the other. Obviously, there’s ample disagreement amongst all scientific groups, including myself.
Oh yeah, I don’t agree with either the AREDS investigators, or with Awh’s group – at least in terms of overall findings, impression, and recommendations. That’s coming up shortly.
But perhaps you’re still thinking that you want the genetic testing in order to best determine which, if any, supplements would be best? Or is it possible that no supplements would be best?
Interestingly, just to make decisions a little more difficult (or easier, depending on your perspective), in May of 2017, the Centers for Medicare and Medicaid Services (CMS) gave conditional approval for reimbursement of so-called pharmacogenetic testing for patients who have AMD. This, despite the fact that another “arm” of the government, the National Institutes of Health (NIH), which was indeed the entity behind the AREDS trial, recommended that genetic testing not be routinely conducted. But, that isn’t the end of this story.
At the time of this writing, I have been informed that, although the Centers for Medicare and Medicaid Services (CMS) has created and approved a CPT code for reimbursement of the genetic testing for AMD patients who already have the disease, the NIH has balked and the code is not currently being reimbursed.
So even if you want the genetic testing, you’ll pay for it out of your own pocket.
And as it turns out, ophthalmologist Carl Awh, MD, the lead investigator and author of the studies assessing genetics and (AREDS) supplements for AMD, is an equity owner and scientific advisory board member of ArcticDx Inc., the very company behind the genetic testing for AMD. This should not influence our consideration for the testing, but I felt it only just that I should submit for your consideration, his financial disclosure, which is required by the journals, and which is part and parcel of his scientific published papers.
Arctic Diagnostics, Genetic Testing, and Supplements
Since introducing my hypothesis regarding the cause (and treatment) of macular degeneration, in August, 2016 at the Ancestral Health Symposium – 2016, which was held at the University of Colorado Boulder, I’ve had numerous speaking engagements around the United States. For many of those speaking engagements, I’ve shared the stage with either Greg Hines, President and CEO of ArcticDx, or with Gerry Belgraver, another representative of ArcticDx. This is the case, because we’re all three regularly invited speakers for the Macular Degeneration Association (MDA) (MacularHope.org).
Quite honestly, I like both of these guys. I’ve even had lunch with Gerry Belgraver, after one of the MDA conferences. However, my hypothesis, supportive research, and treatment recommendations, are all diametrically opposed to that of ArcticDx – and these gentlemen know that. Nevertheless, I sent an email to CEO Greg Hines, and he gave me permission to share the data and tables that they present, both in their live conferences, and on their website (ArcticDx.com).
Again, we must return to the research of Carl Awh and colleagues, which, as you now know, is founded and supported by ArcticDx. In order to understand all this data regarding the genetics of AMD, with their associated supplement recommendations, we must understand a bit of the nomenclature that they use.
So this is not hard – because it’s all based on those two genes: CFH and ARMS2. Those genes, again, are the two that have by far the greatest impact on AMD risk. Well, at least as far as orthodox ophthalmology and ArcticDx is concerned. We’ll get to my position, soon.
Remember that we get two alleles (genes) from each parent – and that we can either have none, one, or two copies of each allele? So ArcticDx makes the following designation for each gene: If you have no copies of the risky CFH gene, that’s coded as “C0.” If you have one copy of the gene, that’s “C1,” and if you have two copies of the gene, that’s “C2.”
And the same goes for the ARMS2 risky gene. If you have no copies of the gene that carries the risk, that’s “A0.” If you have one copy, that’s “A1,” and if you have two copies, that is “A2.”
Got it? So, from their website, in review of some of this research, they state, “The data demonstrated that even though most patients benefitted from AREDS [supplements], for 13% of patients with a specific genetic profile (2 high-risk CFH alleles and 0 ARMS2 risk alleles) the standard AREDS formula was detrimental and accelerated vision loss much faster than placebo.” [71] The latter genetic profile, that is, 2 of the high-risk CFH alleles and none of the ARMS2 risk alleles, would be encoded as “C2A0.” Make sense?
The data from Awh and ArcticDx, based on their analysis of the AREDS study data, finds that the AREDS formula was beneficial in 69% of patients. In the other 31% of patients, the effect of the AREDS formula was actually harmful. For those with the C2A0 genetic profile, there was a 78% increased progression to advanced AMD, with associated vision loss, as compared to placebo. Here’s their table (courtesy of ArcticDx):
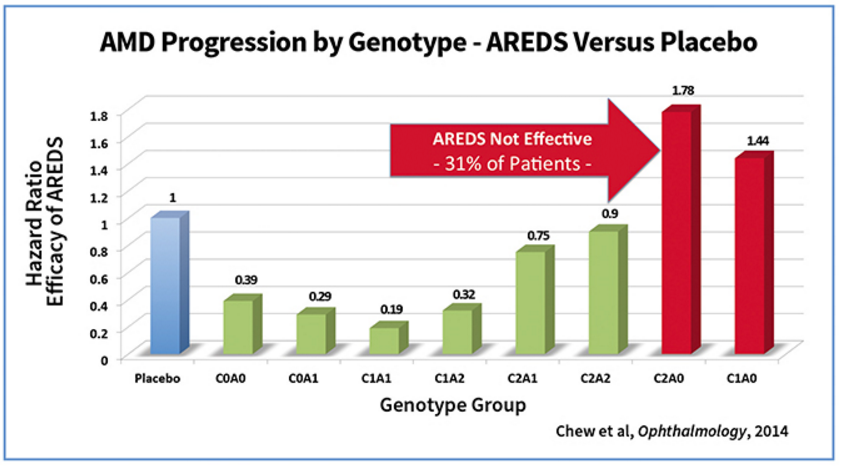
For those who are not graph/table savvy, the above data shows, for example, that those with the C1A1 genetic profile, had an AMD progression that was .19 (19%) the rate of those given placebo, versus those in the C2A0 category, who progressed at a rate 1.78 times faster than those in the placebo category.
ArcticDx did the same thing for the study cited above, by Dr. Seddon and colleagues (2016) along with that of Dr. Awh and colleagues (2015). Once again, here is their table:
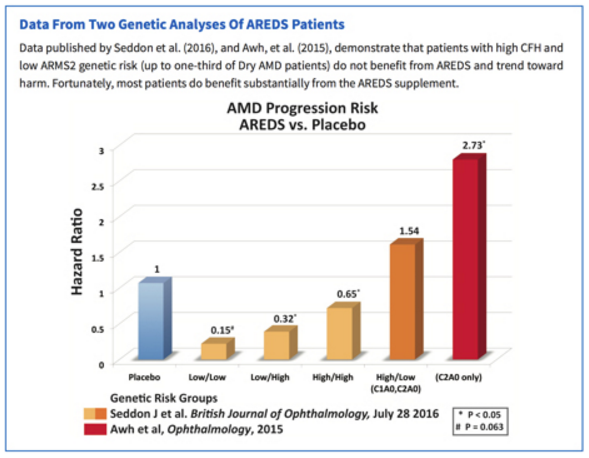
In this table, once again the designations are in reference to the CFH and ARMS2 genetic profiles, so those designated as “Low/Low” may have no CFH risk alleles and no ARMS2 risk alleles, whereas those designated as “High/Low,” as you can see, could either have the C1A0 profile or the C2A0 profile.
In this particular analysis, the “Low/Low” risk group, when given the AREDS formula, only progressed 0.15 times as fast (15%) as those given placebo. And this was statistically significant (1.0).
The conclusion of all of this, is that in the original AREDS study, we know that only 1 out of 13 (8%) patients had a beneficial result. Dr. Awh and colleagues, along with the ArcticDx team, holds that “this is a blended result for all patients – some patients who benefit and some patients who don’t.” (71)
So What’s Wrong With the AREDS Trial and With Awh’s Research?
Well, I’m so glad you asked! Finally, we get to the problems with these studies – and what I’ve been itching to tell you all along.
The primary problem with the AREDS studies and all related investigations is that — Diet Was Never Part of the Analysis.
It’s worth repeating. Diet was never part of the analysis.
This is so extraordinarily important, I’d like to repeat the above message, three more times in a row. But, I’ll spare you.
The AREDS investigators – as well as all the researchers who followed with additional analyses and re-analyses, at best, may have barely mentioned that diet might play any role in AMD development or progression.
And ironically, the treatment that was given to the AREDS participants, i.e., at least those in the experimental (non-placebo) groups, is intended to be a little fragment of a healthy diet. The reality is that, as we’ve reviewed, multivitamin/mineral formulas cause us to be a little less healthy and result in our earlier demise, at least on the whole.
And what is the secondary problem, you ask? Well, this is not an issue with the AREDS studies themselves, or with the re-analyses, but rather with almost every single study related to macular degeneration thus far.
More than 99.9% of the available studies have never looked at entire diets in relation to AMD disease prevalence.
Let’s use an analogy. If you’re trying to determine the cause of lung cancer and you have no idea what the cause is, wouldn’t you want to study both populations that have the disease, as well as those that don’t?
If 10% of the population you’re studying has lung cancer, and they all consume essentially the same diet and 75% of them smoke, hypothetically, wouldn’t you be interested in comparing a population where 0.1% of the population had lung cancer, regardless of what else you knew about them?
Wouldn’t the latter population with 0.1% prevalence of lung cancer, perhaps tell you something about the cause of the dreaded disease? And wouldn’t it make sense to compare this population, in great detail, to the population that had the 10% prevalence of lung cancer, which is 100-fold greater?
This is exactly the scenario that I’m referring to with our treatment of macular degeneration, which is based on the AREDS formulae and associated studies. In general, almost no one has dared to ask the following question:
“In what populations is macular degeneration a medical rarity, and what are they doing differently? What are they eating?”
These are exactly the questions I asked of myself back in 2014.
Undoubtedly, in the late 1920s, Weston A. Price, whom I referred to earlier, asked himself similar questions. Although his interest was in dental decay and general physical degeneration, he set out to determine what was different about the diets of people who did not develop those conditions.
Price knew that, even in the 1920’s, he could not find an appropriate “control group” in the United States, i.e., people who were not consuming the “experimental diet” (Westernized, man-made, nutrient-deficient, and even toxic foods). Even by the 1920s, people in the United States were already consuming substantial amounts of refined white flour, sugar, canned goods, sweets, vegetable oils, and trans fats. I’ve reviewed this extensively in my book, briefly in the Introduction article on this site, and briefly in most of my live presentations.
Instead of spending decades and millions of dollars studying dental decay and general physical degenerative diseases, such as heart disease, cancer, arthritis, etc., in those people who were already severely afflicted, which is what almost all current studies have done, Price set out to study populations all around the world who did not have these diseases.
The end results, of course, were astonishing. Price discovered that numerous degenerative diseases followed the introduction of Westernized, processed, nutrient-deficient dietary components in significant quantities.
He found, on the contrary, that those who continued to consume their native, traditional, nutrient-dense diets, remained in brilliant health and without degenerative conditions.
Let me remind you: Age-related Macular Degeneration, as its name implies, is a degenerative disease.
For those not aware, in 2013, I hypothesized the following: “The ‘displacing foods of modern commerce’ are the primary and proximate cause of age-related macular degeneration.” We’ve researched this hypothesis, through correlative data, assessing the consumption of the ‘displacing foods’ versus AMD prevalence, in 25 nations. This data, strongly supports the hypothesis that the ‘displacing foods of modern commerce,’ are indeed the cause of AMD.
Next, we’ll look at just a couple of the 25 nations where we ran these correlative studies.
Where Macular Degeneration is Rarely Found…
In attempt to follow in Weston Price’s footsteps, in early 2015, I set out to try to determine if macular degeneration was confirmed to be rare in any regions, anywhere in the world. What I found was that, in almost all populations where macular degeneration prevalence had been formally assessed by scientific analysis, the prevalence in recent decades was generally found to be high – often between 20% and about 40%, for those above age 75 to 80. But, let me cite a couple formal studies, to keep this scientific.
Globally, for people between the ages of 45 and 85 years of age, 8.69% have some degree of AMD.[72] In the U.S. Beaver Dam Eye Study, conducted between 1988 to 2005 and ongoing, for those aged 43 to 54, AMD affected 8.4%, ages 55 to 64, 13.8% were affected, ages 65 to 74, 18.0% affected, and for those 75 and older, a whopping 29.7% were affected with AMD.[73]
Without getting into the nitty-gritty detail, in late 2015 and early 2016, I made contact with ophthalmologists in some of the Pacific Island nations. In great contrast to the epidemics of AMD in virtually every developed nation where formal AMD studies have been completed, the prevalence of macular degeneration in the Pacific Island nations of Samoa, Solomon Islands, and Kiribati, is approximately 0.2%, and perhaps even less. This prevalence holds true for people over the age of 60 and into the elderly years.
This is an astonishingly low prevalence of AMD, confirmed by chart reviews via the ophthalmologists of these three nations. In fact, in comparing the prevalence of AMD for the approximate same age categories between nations, the U.S. has approximately 74-fold greater prevalence of AMD if compared to Samoa, Solomon Islands, and Kiribati.
Below is our graph for the Solomon Islands, with the proxy-processed food markers of sugar and vegetable oils, plotted against AMD prevalence.
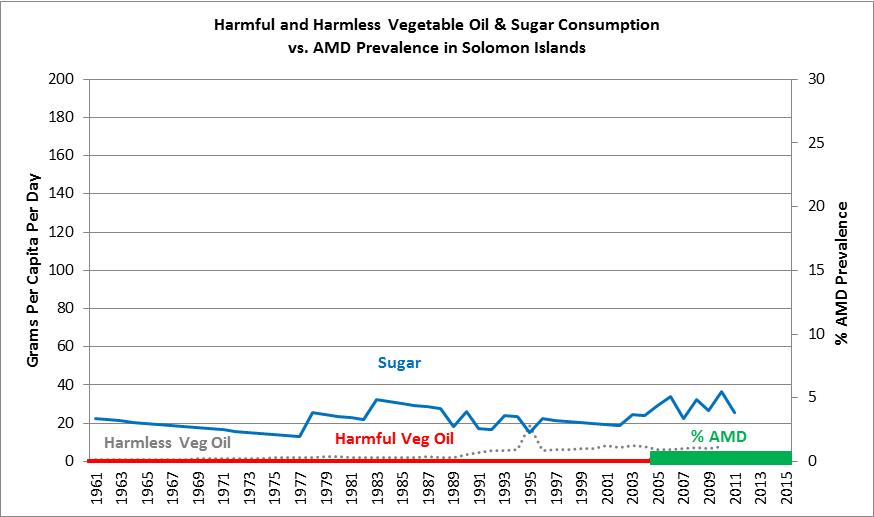
Once we analyzed the diets of these nations, it was clear that, this is almost precisely what the hypothesis would have predicted, with the exception of a surprising finding in Kiribati. The consumption of sugar, a proxy marker for processed food, was extremely low in the Solomon Islands, moderately low in Samoa, and moderately high in Kiribati. However, the polyunsaturated (‘harmful”) vegetable oil consumption, which is also a strong proxy marker of processed food consumption, was essentially zero in all three nations, since 1961, as evidenced by data from the Food and Agriculture Organization of the United Nations (FAO).[74]
In general, these are some of the few populations on the planet that have been consuming largely native, traditional diets over a significant part of the past 60 years. This is evidenced by the fact that the majority of the Pacific Island Nations and Territories (PICTs) have relied almost entirely on fish and seafood for their protein sources, along with a quite large variety of roots and tubers, i.e., complex carbohydrates.[75] Traditionally, the roots and tubers consumed by Pacific Islanders have included taro, sweet potatoes, and yams, and they’ve also traditionally consumed a large variety of tropical fruits that were eaten in large quantities, including bananas, plantains, mangoes, papayas, and pineapples.[76]
The coconut is a major subsistence crop in the Pacific Island nations, where every edible part of the coconut is eaten, including a substantial reliance on coconut milk and coconut oil.[77]
Hughes and Lawrence of the University of Queensland, Brisbane, Australia, have shown that many of the PICTs have experienced Westernization of the diet in more recent decades, as evidenced by increasing reliance and consumption of commercialized, nutrient-deficient, imported foods.[78] These foods are primarily being imported from Australia, New Zealand, and the USA, all of which have been accused of food “dumping,” with allegations relating to poor nutrition quality. This, of course, has been followed by a severe overall decline in the health of Pacific Islanders, with dramatically increasing rates of obesity, communicable, and non-communicable diseases.(78)
In the island nations of Solomon Islands, Samoa, and Kiribati, however, the transition to Westernized diets has obviously not occurred to the extent that it has in many other Pacific Islanders (their sugar and vegetable oil consumption data confirm by FAO) and, as such, they’ve not succumbed to many of the chronic, degenerative diseases that take at least a few decades to develop, such as heart disease and macular degeneration.
“The fate of nations is determined by what they eat.”
— Jean Anthelme Brillat-Savarin (1825)
When the prevalence of AMD was once found to be low in various populations, such as the Japanese people (of Japan), the assertion was made that the Japanese were “genetically protected.” In fact, I recall this assertion in regards to the Japanese (again, of Japan) when I was a resident in ophthalmology at the University of Colorado Health Sciences Center, in Denver, in the years 1991 – 1994.
This assertion, i.e., that races and cultures are “genetically protected,” is what those of us in ancestral nutrition now refer to as “playing the genetics card.” This, of course, is the incorrect and inchoate belief system that people are protected from degenerative diseases based purely on their genetic constitution. No doubt, we all have genetic predispositions, but Price’s treatise on this subject, Nutrition and Physical Degeneration, left no doubt that not a single racial or cultural group can retain immunity to the ravages of nutrient-deficient, processed food-laden diets. People of every race, ethnicity, or cultural heritage are at risk – and of course – this is only logical.
Why should we expect that anyone, of any given race, should be immune to the ravages of nutrient-deficient diets, replete with toxic components?
With regard to AMD prevalence in Japan, between the years 1974 and 1979, at the Nagoya University Hospital, in Nagoya, Japan, only 24 eyes with dry macular degeneration and 36 eyes with wet macular degeneration were found among 31,334 outpatient visits during that period. By estimating that 90% of those seeking eyecare were over age 40, which is quite typical (remember, these are people visiting a hospital for eyecare, not an outpatient optometry clinic), this leaves 60 patients affected by AMD, out of some 28,201 total patient visits, for an approximate prevalence of 0.2%. This assumes only one patient represents each eye affected, which is highly unlikely and would, therefore, make the prevalence of AMD during that period potentially even lower.
Less than 30 years later, in 2007, the Hisayama Study in Japan found that, of residents age 50 and above, 10.0% had early AMD and 1.4% had late AMD, for a total AMD prevalence of 11.4%.[79]
And just in case we might think that the Hisayama Study was a fluke, an unusual population, or in any other way non-representative of rising AMD prevalence in Japan, in 2013, the Nagahama Study in Japan found early AMD prevalence of 16.1% in the 50 to 59 year-old category, and 31.2% in the 70 to 74 year-old category.[80] In this same study, advanced AMD was present in 0.27% of the 50 to 59 year-olds and 0.98% of the 70 to 74 year-olds.
If we only compare the prevalence of AMD in the late 1970s to that of the 2007 Hisayama study in Japan, this is a staggering 57-fold increase in the prevalence of AMD, in a span of just 30 years. This cannot possibly be explained by genetics – or aging of the population.
There are multiple other large population examples of the AMD prevalence most definitely rising in such time periods, which I’ve reviewed (once again) in the Introduction, and in my book.
The question is – what could possibly induce a 57-fold increase in the prevalence of AMD, in Japan, in just 30 years?
The answer, of course, is Westernization of the diet. And we have the data to prove it – see the graph below.
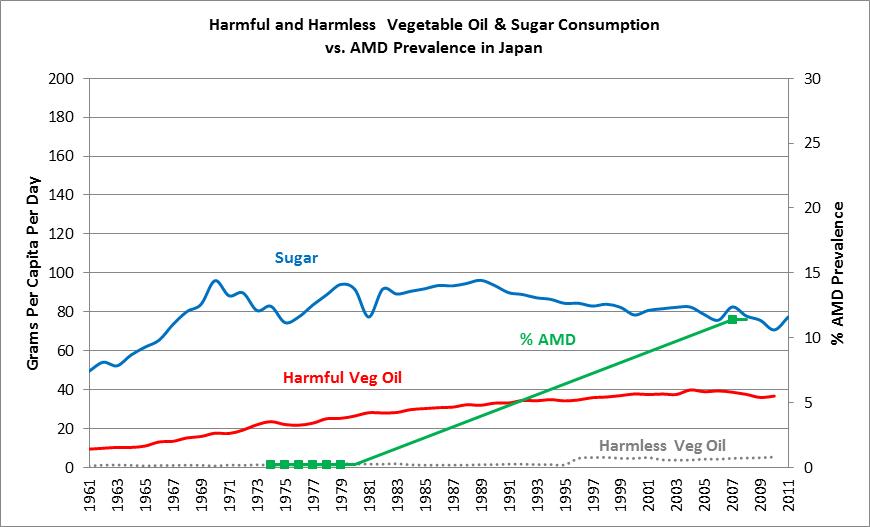
Once again, if we examine sugar consumption, a well-known proxy-marker of processed food consumption, we see that consumption in Japan in 1961 was roughly 50 grams per day, and subsequently rose to 80 to 90 grams per day in succeeding decades. The “harmful vegetable oils,” which are those containing significant polyunsaturated oils, rose from 9 grams per day in 1961, to 40 grams per day by 2003, which is a 4.5-fold increase in the consumption of these dangerous vegetable oils. This, of course, indicates a dramatic increase in the consumption of Westernized, processed, nutrient-deficient foods, in this short period of time.
And the consequences? Well, a drastic increase in “diseases of Western civilization,” including obesity, hypertension, metabolic syndrome and, of course, macular degeneration, as reviewed above.
Here’s a typical headline – and this one happens to come from the japan times.
This one from GoodFoodWorld.com…
![]()
And this one from CNN.com…
Furthermore, a great deal of research has focused on the fact that the Japanese have developed a drastically higher prevalence of chronic, metabolic diseases, primarily over the past four decades. For example, a paper published in the Asia Pacific Journal of Clinical Nutrition, in 2002, duly noted this drastic increase in chronic, metabolic diseases in Japan. They wrote that the Japanese have experienced a “rapid increase in incidence of obesity-associated chronic diseases such as diabetes, hypertension and hyperlipidemia [abnormal blood lipids].” [81]
And because Asians generally have very lean and “slim” physiques, the Japan Society for the Study of Obesity (JASSO) determined that it was more appropriate to define obesity as Body Mass Index (BMI) of greater than or equal to 25 (kg/m2), rather than the U.S. cut-off, of 30.(81) Given this criteria, the same study found that, in the forty-year period between approximately 1962 and 2002, obesity prevalence in Japan increased four-fold in men over 30 years old and three-fold in women over 40 years of age.81 And at the time of this study (2002), obesity in the Japanese was at an all-time high of 20 percent.(81)
And in the last 40 to 50 years, numerous Western fast-food restaurants have populated Japan…

In nation after nation, population after population, the people Westernize their diets with the likes of refined white flour, refined (added) sugars, polyunsaturated vegetable oils, and trans fats, which all come from man-made, processed, nutrient-deficient, and even toxic food components. Yes, toxic. Then, within a few years, the people are becoming ill. They’re developing dental decay, children grow up with crooked teeth, cavities develop, and even dental abscesses (in adults, generally), which is then followed by other chronic, degenerative diseases, including type 2 diabetes, hypertension (high blood pressure), metabolic syndrome (visceral obesity, abnormal blood lipids, insulin resistance/pre-diabetes), overweight and obesity, even the autoimmune diseases (like rheumatoid arthritis, lupus, multiple sclerosis, etc.), then cancers of epithelial origin primarily, and finally, heart disease, strokes, Alzheimer’s disease, dementia, and more… And then the governments, major preventive healthcare entities, healthcare dictocrats, and scientists seem to be scratching their heads, wondering what happened.
Of course, now we have the data to support the hypothesis that AMD is caused by the exact same thing, i.e., man-made, processed, nutrient-deficient and toxic diets, which not only lead to all of this chronic, metabolic disease, but to AMD as well.
As previously alluded to, our scientific paper on this research is now published in the prestigious journal, Medical Hypotheses, which is an Elsevier, peer-reviewed publication. My colleague and co-author in this research, Marija Stojanoska, MSc, from Macedonia, are extremely proud of this paper, which for me at least, was six years in the making…
To access our paper at the journal online, Click Here.
With that understanding…
Now that we’re (hopefully) a little closer to “being on the same page,” let’s return to the research submitted by Carl Awh, MD and ArcticDx, regarding their data…
Despite all of the contention regarding Awh’s research, I believe that there is merit to their position that genetics does indeed play a role in regard to either the benefits or the harm, caused by the AREDS synthetic vitamin formulae. And indeed, as you may recall, Johanna Seddon, MD, of Tufts University in Boston, who has contributed more towards nutrition and AMD over the last 25 years than probably any other previous researcher, also found and agreed that genetics is important in supplementation decisions. To reiterate, her paper stated, “The effectiveness of antioxidant and zinc supplementation appears to differ by genotype. Further study is needed to determine the biological basis for this interaction.” (70)
So where is the big problem, you ask?
Recall that I previously intimated that the single greatest problem with the AREDS study and data – is that there was no consideration or analysis of diets? And if I didn’t come right out and say it, did I mention that this is really an oversight of colossal proportions?
Once again, this is the case, because the entire cohort of participants for the study was drawn from the U.S. population. And guess what the enormous majority of the population in the U.S. is consuming for a diet?
The answer? The Standard American Diet (SAD), with the appropriately named acronym.
We know, as previously reviewed, that at least 63% of the American (U.S.) diet is composed of refined grains (mostly wheat), refined and added sugars, polyunsaturated vegetable oils, and trans fats, right? And please recall that these are almost entirely nutrient-deficient foods.
So the so-called “Placebo” group, which received pills of no consequence, were already in the experimental group, right?
In other words, they’re already consuming the very diet that, as Marija Stojonoska and I have shown, is associated with macular degeneration development in the first place.
We know this – well – if you were to review all of our data and correlations from 25 nations – and so, if we compare the U.S. population’s risk of AMD to that of the Pacific Islanders from either the Solomon Islands, Samoa, or Kiribati, then we understand that the approximate, relative risk of developing AMD in the U.S., compared to these three island nations, is 74-fold greater.
Knowing this, we can rename the “Placebo” group in the AREDS trial histogram (table) as the “SAD” group, and instead of assigning their relative risk as 1.0, as the ArcticDx group did, we can assign their risk as 74 – because the risk in the SAD group from the U.S. is 74-fold greater than those consuming a relatively native, traditional (Ancestral) diet, in the Solomon Islands, for example, whose relative risk would then be 1.
In other words, the U.S. diet (SAD) causes relative risk of AMD that is 74-fold greater than an ancestral diet (let’s call this category, “Ancestral Diet”), practiced in the Pacific Island nations (Solomon Islands, Samoa, and Kiribati) studied, right?
Now, let’s look at the data again, and re-plot the data with the “SAD” group at relative risk of 74, and the “Ancestral” group at relative risk of 1. Next, we’ll throw in the genetic and supplement categories, re-assigned with their respective risk based on genetics and consumption of the AREDS vitamin/mineral formula. Now what we have is this…
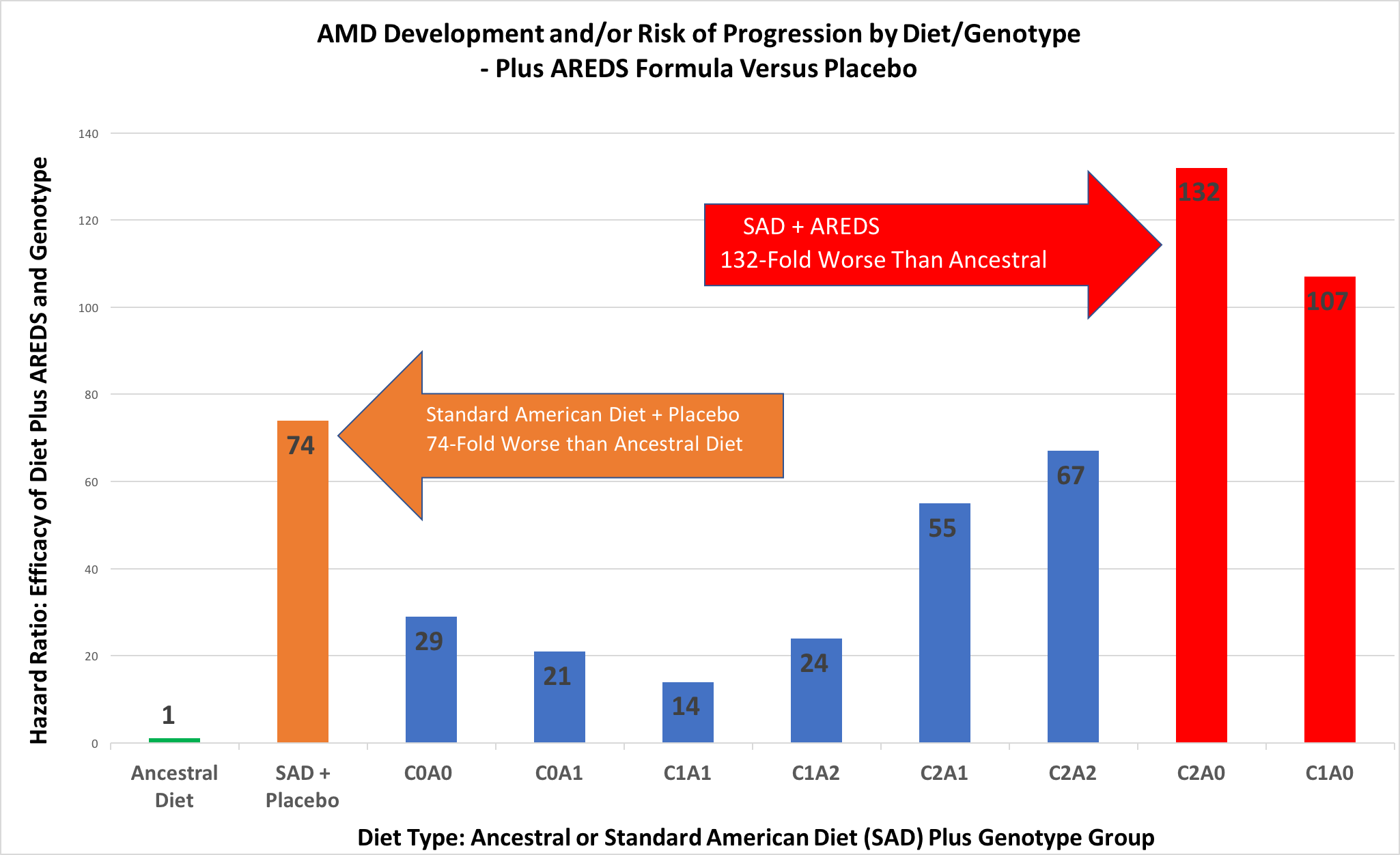
For me, a picture (or graph) is worth a thousand words. But, I know this isn’t the case for everyone. So for those who want the explanation in words, here goes…
If we look at the “Ancestral Diet” category, we see that the relative risk of developing AMD is 1.0, as compared to the Standard American Diet (SAD), which is 74. Alternatively stated, as compared to the Ancestral Diet, the relative risk of developing AMD with the SAD diet is 74-fold greater.
Now, in the best possible scenario, for the segment of the population that has the C1A1 genetic combination, which was 22.6% of the population,(55) if you consumed the SAD diet and took the AREDS formula, your risk of progression of AMD was approximately 14-fold higher than those in the “Ancestral Diet” group. This is the best possible scenario if you’re consuming the SAD diet, have the “best” genetic profile, and consume the AREDS formula regularly.
In the worst-case scenario, for those who have the C2A0 genetic combination, which was 13.2% of the population, and who also consume the SAD diet and take the AREDS formula,(55) the risk of AMD progression for that category is 132-fold greater, approximately, than those people consuming the “Ancestral Diet.”
So to summarize, if you’re consuming the SAD diet and take the AREDS formula, in the best possible circumstances, your risk of AMD development/progression is about 14-fold higher than if you consumed an Ancestral Diet. In the worst-case scenario, if you’re consuming the SAD diet and take the AREDS formula, your risk of AMD development/progression is about 132-fold greater than if you consume an Ancestral Diet.
Surely this makes the decision a “no-brainer,” right?
Conclusion: Which Are the “Best Eye Vitamins”?
In a nutshell, the answer to this question is that the “best eye vitamins” are the vitamins contained in ancestral diets, that is, those vitamins contained in whole, natural, unprocessed foods, of both plant and animal origin, and which are preferably organic in nature.
Only in whole foods are the vitamins in the right proportions and context, associated with all the correct co-factors including minerals, enzymes, phytonutrients, polyphenols, etc., and the most bio-available.
But let’s ask and answer several questions based on this article and the data presented…
First, which is better: the Standard American Diet (SAD, or Westernized diet) or an Ancestral Diet, in terms of preventing AMD?
The answer: Based on our research, the risk of AMD development is approximately 74-fold higher with the SAD/Westernized diet versus an ancestral diet, at least if we’re comparing the U.S. data to that of the Pacific Islanders studied.
Second, which is better in terms of preventing AMD development/progression: the SAD diet plus AREDS formula supplements, or the Ancestral Diet?
The answer: Based on our research, in the best possible scenario (for those consuming a SAD diet), the Ancestral Diet is still 14-fold better, and in the worst possible scenario, the SAD (Westernized) diet is 132-fold worse than an ancestral diet.
Third, should vitamin supplements, such as the AREDS formulae, be the primary focus of treatment for dry AMD?
The answer: Absolutely not. Not even close. In my opinion, synthetic vitamin supplements should generally not be consumed, except in unusual circumstances.
In general, one absolutely must remember that the synthetic multivitamins are likely to make your health worse and cause your earlier demise. This is a fact, proven by the Cochrane meta-analyses – and is inarguable.
Keep in mind that the AREDS formula is a multivitamin. Perhaps worst of all, consuming these might make you think you’re doing something good while you continue to consume the very foods that caused your AMD in the first place (if indeed you do already have AMD).
So are vitamins important in preventing AMD?
Yes, absolutely. In fact, tremendously so. However, the AREDS supplement likely doesn’t even provide the vitamins most important to preventing AMD, which, based on our research, are the fat-soluble vitamins. Those most likely to play major roles in AMD development (or prevention, as the case may be) include vitamins A, D, and K2. This is yet another entirely separate subject matter, and is covered in detail only in my book at this point.
However, one should realize that, as reviewed in my book, the PUFA vegetable oils, trans fats, and possibly sugar, all appear to have direct toxicities in the development and evolution of AMD, plus they displace nutrient-dense foods, such as pasture raised meats, fish and seafood, pastured eggs, butter from pastured cows, raw milk, organically grown fruits and vegetables, and organically grown grains that are properly prepared (soaked, fermented, or sprouted).
Perhaps even more important are the “sacred foods.” These are the foods that are particularly rich in the fat-soluble vitamins (A, D and K2 particularly), and which every healthy, traditional living society of which Price studied, somehow knew through what Price referred to as “accumulated wisdom,” would make for healthy babies, would prevent physical degeneration and many diseases, including infectious diseases, and in general would allow for healthy minds and bodies. These particular foods consisted of butter from cows grazing on green grass (pastured butter), whole, raw milk, organ meats such as liver, heart, kidneys, pancreas, etc., fish and other seafood, and fish eggs (roe).
A centuries old tradition, which might certainly be considered a sacred food (primarily in Western societies), is also extra virgin cod liver oil (EVCLO), which is not a supplement, but rather a whole food that comes straight from the livers of fish. This is a fantastic source of both vitamin A and vitamin D, of which most people are currently severely lacking. For those not regularly consuming the liver of terrestrial animals (beef and chicken, for example, which are great sources of vitamin A) along with either lots of fatty fish and seafood (e.g., salmon, herring, mackerel, and sardines, all of which are good sources of vitamin D) or sunshine (another great source of vitamin D), then EVCLO is a fantastic substitute. I strongly recommend this for those not regularly consuming organ meats as well as lots of fatty fish and seafood, and who don’t regularly get good sun exposure to bare skin (plus one has to be at the “right” latitude, at mid-day, and at the right time of year to properly convert vitamin D).
Also, I promised that I would return to the issue that these antioxidant multivitamins used in studies do not prevent AMD in the first place, and yet are expected to prevent progression once the disease has begun.
Again, is this just a paradox?
I would assert that it is not entirely a paradox. In fact, I believe there is a logical conclusion here. The antioxidant vitamins, which at least in pill form have shown no benefit to preventing AMD, could potentially help prevent AMD progression once the disease is moderate or severe (as the AREDS study found).
Why would this be the case? Because, very potentially, those that already have moderate or severely advanced AMD also have the worst nutritional status! These are the people, who have generally continued their SAD (or Westernized) diets for a number of additional years beyond when they had grade 1 or 2 (early) AMD, further depleting nutrient and even antioxidant stores. In this scenario, even the marginally beneficial AREDS formula may benefit people in such severely malnourished states.
The question to ask is in this scenario is not “What would be marginally beneficial?” But rather, “What is the most optimal nutrition?”
Once again then, which are the “best eye vitamins”? Well, they are those that are in whole, natural, entirely un-processed, ancestral diets. And preferably organic. And these diets must include animal sources in order to properly supply the fat-soluble vitamins in sufficient quantities.
As Weston A. Price discovered, all vibrantly healthy, happy, disease-free societies that he found were consuming animal foods. In some cases, such as certain African tribes, these animal sources primarily came from insects. But, they did indeed have animal sources to supply these vitamins.
Secondly, all of the healthy groups that Price found were not consuming refined white wheat flour, added sugars, sweets, confectionary, canned goods, and vegetable oils.
I’ve re-organized these categories of “foods” to be avoided as:
- Refined white wheat flour
- Refined (added) sugars
- Polyunsaturated vegetable oils
- Artificially created trans-fats (hydrogenated and partially hydrogenated vegetable oils)
Based on the hypothesis I’ve proffered and the supportive research that my colleague, Marija Stojanoska, and I have completed, we have asserted that the term “Age-Related Macular Degeneration” should be replaced and supplanted by the more appropriate term, “Diet-Related Macular Degeneration,” or DMD. We believe this will place the focus of prevention – and treatment – on the true underlying cause.
We hope you agree.
I’ll end this article with a quote from the man, the scientist, the researcher, and the dentist, whom many have referred to as the “Isaac Newton of Nutrition,” who not only completed an epic work of nutritional anthropology, but who published those works in his treatise, Nutrition and Physical Degeneration (1939). In this timeless book, which presented revolutionary research that could never again be completed, Price wrote,
“Great harm is done, in my judgment, by the sale and use of substitutes for natural foods.” [82]
— Weston A. Price
I couldn’t agree more.
In my opinion, if you only read one book on nutrition in your lifetime, don’t read mine. Read Weston A. Price’s book, Nutrition and Physical Degeneration, available at PPNF.org.
This article was written by Ophthalmologist, Chris A. Knobbe, MD
Associate Clinical Professor Emeritus
University of Texas Southwestern Medical Center – Dallas
Founder & President, Cure AMD Foundation™
Dr. Knobbe would like to thank Andrew J. Luff, MA, MB, BS, FRCS, FRCOphth, Vitreo-Retinal surgeon from the U.K., for his assistance in the AREDS study data and analysis.
REFERENCES
- Knobbe, Chris A. Ancestral Dietary Strategy to Prevent and Treat Macular Degeneration. Vervante, Springville, Utah, 2016, pp. 14-29. ↑
- Ibid. pp. 104 – 137. ↑
- Albert, Daniel M. The History of Ophthalmology. Blackwell Science, Inc., Cambridge, Massachusetts, 1996, p. 76. ↑
- Albert, Daniel M., Edwards, Diane D. The History of Ophthalmology. Cambridge, Massachusetts, Blackwell Science, 1996. p. 195-196. ↑
- Klein R, Klein BE, Linton KL. Prevalence of age-related maculopathy. The Beaver Dam Eye Study. Ophthalmology. 1992; 99: 933-943. ↑
- Hutchinson J, Tay W. Symmetrical central choroido-retinal disease occurring in senile persons. R Lond Ophthalmic Hosp Rep J Ophthalmic Surg. 1874; 8: 231-244. ↑
- Keeler CR. A Brief History of the Ophthalmoscope. The Royal College of Ophthalmologists, London, UK, Accepted for publication 16 June 2003. Available at: Optometry in Practice 2003; Vol 4: 137-145. ↑
- Fuchs, Ernest. Textbook of Ophthalmology. New York, D. Appleton and Company, 1892. p. 315. ↑
- Fuchs, Ernest. Textbook of Ophthalmology. New York, D. Appleton and Company, 1892. pp. 257-264. ↑
- Haab O. Erkrankungen der Macula Lutea. Diseases of the macula lutea. Centralblatt für praktische Augenheilkunde. 1885(9): 383-4. ↑
- Haab O. Ueber die Erkrankung der Macula lutea. On the disease of the macula lutea. Siebenter Periodischer Internationaler Ophthalmologen-Congress Heidelberg. 1888, p. 429. ↑
- Klein R, Klein BEK, Cruickshanks KJ. The Prevalence of Age-Related Maculopathy by Geographic Region and Ethnicity. Progress in Retinal and Eye Research. 1999;18(3):371-389. ↑
- Knobbe, Chris A. Ancestral Dietary Strategy to Prevent and Treat Macular Degeneration. Vervante, Springville, Utah, 2016, pp. 14-29. ↑
- Duke-Elder, W. Stewart. Recent Advances in Ophthalmology. Philadelphia, P. Blakiston’s Son & Co., 1927. p. XV. ↑
- Duke-Elder, WS. Textbook of Ophthalmology – Duke-Elder, Vol. III, Diseases of the Inner Eye. St. Louis: The C.V. Mosby Company, 1940. p. 2372. ↑
- Duke-Elder, WS. System of Ophthalmology. Vol IX Diseases of the Uveal Tract. St. Louis: The C.V. Mosby Company, 1966. pp. 609-614. ↑
- Kahn HA, Leibowitz HM, Ganley JP, et al: The Framingham Eye Study II. Association of ophthalmic pathology with single variables previously measured in the Framingham Heart Study. Am J Epidemiol 1977; 106: 33. ↑
- Kahn HA, Leibowitz HM. Ganley JP, et al. The Framingham Eye Study I. Outline and major prevalence findings. Am J Epidemiol. 1977; 106(1): 17-32. ↑
- Kini MM, Leibowitz HM, Colton T, et al. Prevalence of senile cataract, diabetic retinopathy, senile macular degeneration, and open angle glaucoma in the Framingham Eye Study. Am J Ophthalmol. 1978: 85 (1): 28-34. ↑
- Piro A, Tagarelli G, Lagonia P, et al. Casimir Funk: his discovery of the vitamins and their deficiency disorders. Ann Nutr Metab. 2010;57(2):85-8. ↑
- Price, Catherine. Vitamania – Our Obsessive Quest For Nutritional Perfection. Penguin Press, New York, 2015, pp. 27-46. ↑
- Waugh WA, King CG. Isolation and identification of vitamin C. J Biol Chem. 1932, 97: 325-331. ↑
- Wolf G. The Discovery of Vitamin D: The Contribution of Adolf Windaus. J Nutr. 2004; 134(6):1299-1302. ↑
- Goldberger J, Waring CH, Willets DG. The prevention of pellagra: a test of diet among institutionalized inmates. Public Health Rep. 1915: 30: 3117-3131. ↑
- Elvehjem CA, Madden RJ, Strong FM, et al. Relation of nicotinic acid and nicotinic acid amide to canine black tongue. J Am Chem Soc. 1937; 59: 1767-1768. ↑
- Price, Catherine. Vitamania – Our Obsessive Quest For Nutritional Perfection. Penguin Press, New York, 2015, pp. 1-11. ↑
- Price, Catherine. Vitamania – Our Obsessive Quest For Nutritional Perfection. Penguin Press, New York, 2015. ↑
- Bishai D, Nalubola R. The History of Food Fortification in the United States: Its Relevance for Current Fortification Efforts in Developing Countries. Economic Development and Cultural Changes. 2002;51(1): 37-53. ↑
- Fulgoni VL, Keast DR, et al. Foods, Fortificants, and Supplements: Where Do Americans Get Their Nutrients? J Nutr. 2011; 141: 1847-1854. ↑
- USDA Economic Research Service. U.S. Food Consumption as a Percent of Calories – 2009. Available at: http://www.ers.usda.gov. ↑
- Price, Weston A. Nutrition and Physical Degeneration. Lemon Grove, California, The Price-Pottenger Nutrition Foundation, Inc., 1939. ↑
- Price, Weston A. Nutrition and Physical Degeneration. Lemon Grove, California, The Price-Pottenger Nutrition Foundation, Inc., 1939, p. xvi. ↑
- Price, Weston A. Nutrition and Physical Degeneration. Lemon Grove, California, The Price-Pottenger Nutrition Foundation, Inc., 1939, p. 246-248, 452. ↑
- Cordain L. Implications of Plio-Pleistocene hominin diets for modern humans. In: Ungar P, editor. Evolution of the Human Diet: The Known, the Unknown, and the Unknowable. New York: Oxford University Press; 2007: 363-383. ↑
- Cordain L, Eaton SB, Sebastian A, et al. Origins and evolution of the Western diet: health implications for the 21st century. Am J Clin Nutr 2005; 81(2): 341-354. ↑
- O’Keefe JH, Cordain L. Cardiovascular Disease Resulting From a Diet and Lifestyle at Odds With Our Paleolithic Genome: How to Become a 21st-Century Hunter-Gatherer. Mayo Clinic Proc 2004; 79:101-108. ↑
- Carrera-Bastos P, Fontes-Villalba M, O’Keefe JH, et al. The western diet and lifestyle and diseases of civilization. Research Reports in Clinical Cardiology 2011; 2: 15-35. ↑
- Goldberg J, Flowerdew G, Smith E, et al. Factors associated with age-related macular degeneration. An analysis of data from the first National Health and Nutrition Examination Survey. Am J Epidemiol. 1988;128(4): 700-10. ↑
- Knobbe, Chris A. Ancestral Dietary Strategy to Prevent and Treat Macular Degeneration. Vervante, Springville, Utah, 2016, pp. 151-161. ↑
- Gomboeva SB, Shumaev KB, Gessler NN, Lankin VZ. The mechanism of oxidation of beta-carotene and polyunsaturated fatty acids. Doklady Biochemistry and Biophysics. 2001;377:98-101. ↑
- Knobbe, Chris A. Ancestral Dietary Strategy to Prevent and Treat Macular Degeneration. Vervante, Springville, Utah, 2016, pp. 65-79. ↑
- Seddon JM, Ajani UA, et al. Dietary carotenoids, vitamins A, C, and E, and advanced age-related macular degeneration. Eye Disease Case-Control Study Group. JAMA. 1994 Nov 9; 272(18): 1413-20. ↑
- Evans JR, Lawrenson JG. Antioxidant vitamin and mineral supplements for preventing age-related macular degeneration (Review). The Cochrane Collaboration. The Cochrane Library, 2012, Issue 6. ↑
- Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol. 2001; 119(10): 1417-36. ↑
- Age-Related Eye Disease Study 2 Research Group. Lutein + zeaxanthin and omega-3 fatty acids for age-related macular degeneration: the Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA. 2013; 309(19): 2005-15. ↑
- Evans JR, Lawrence JG. Antioxidant vitamins and mineral supplements to slow the progression of age-related macular degeneration. Cochrane. 14 Nov 2012. ↑
- Bjelakovic G, Nikolova D, Gluud LL, et al. Antioxidant supplements for prevention of mortality in healthy participants and patients with various diseases. Cochrane Database Syst Rev. 2012;14(3):CD007176. ↑
- Ng T W, Goggin M. Awareness of and compliance with recommended dietary supplement among age-related macular degeneration patients. Clinical & Experimental Ophthalmology. 2006; 34(1):9-14. ↑
- Hochstetler BS, Scott I, Kunselman A, et al. Adherence To Recommendations of the Age-Related Eye Disease Study in Patients With Age-Related Macular Degeneration. Retina. 2010;30(3):1166-1170. ↑
- Age-Related Eye Disease Study 2 Research Group. Lutein + zeaxanthin and omega-3 fatty acids for age-related macular degeneration: the Age-Related Eye Disease Study 2 (AREDS@) randomized clinical trial. JAMA. 2013;309(19): 2005-15. ↑
- Miller ER, Pastor-Barriuso R, Dalal D, et al. Meta-Analysis: High-Dosage Vitamin E Supplementation May Increase All-Cause Mortality. Ann Intern Med. 2005;142(1):37-46. ↑
- Lawlor DA, Smith GD, Bruckdorfer KR, et al. Those confounded vitamins: what can we learn from the differences between observational versus randomized trial evidence? Lancet. 2004;363:1724-27. ↑
- Sesso, Howard. “Demystifying nutrition – The value of food, vitamins and supplements.” The Longwood Seminars. Harvard Medical School. Published Mar 8, 2013. Available at: https://www.youtube.com/watch?v=j9E8bUIEsIo. Accessed Oct 5, 2017. ↑
- Tice, Jeffrey. “Vitamins and Supplements: An Evidence-Based Approach.” University of California Television (UCTV). Published Oct 29, 2013. Available at: https://www.youtube.com/watch?v=2mDrAQi1SwU. ↑
- Awh CC, Lane AM, Hawken S, et al. CFH and ARMS2 genetic polymorphisms predict response to antioxidants and zinc in patients with age-related macular degeneration. Ophthalmology. 2013; 120(11): 2317-23. ↑
- Haines JL, Hauser MA, Schmidt S, et al. Complement factor H variant increases the risk of age-related macular degeneration. Science. 2005; 308(5720):419-421. ↑
- Edwards AO, Ritter R 3rd, Abel KJ, et al. Complement factor H polymorphism and age-related macular degeneration. Science. 2005;308(5720):385-389. ↑
- Hageman GS, Anderson DH, Johnson LV, et al. A common haplotype in the complement regulatory gene factor H (HF1/CFH) predisposes individuals to age-related macular degeneration. Proc Natl Acad Sci USA. 2005;102(20):7227-7232. ↑
- Klein RJ, Zeiss C, Chew EY, at al. Complement factor H polymorphism in age-related macular degeneration. Science. 2005;308(5720):385-389. ↑
- Zareparsi S, Branham KE, Li M, et al. Strong association of the Y402H variant in complement factor H at 1q32 with susceptibility to age-related macular degeneration. Am J Hum Genet. 2005;77(1):149-153. ↑
- Grassman F, Heid IM, Weber BHF. Recombinant haplotypes narrow the ARMS2/HTRA1 association signal for age-related macular degeneration. Genetics. 2017;205(2):919-24. ↑
- Wang G, Scott WK, Agarwal A, et al. Coding variants in ARMS2 and the risk of age-related macular degeneration. JAMA Ophthalmol. 2013;131:1-2. ↑
- Boggs W. Risk Factors Influence Age of Onset of Age-Related Macular Degeneration. Medscape Ophthalmology. March 2, 2015. Available at: www.medscape.com. ↑
- Awh CC, Lane AM, Hawken S, et al. CFH and ARMS2 Genetic Polymorphisms Predict Response to Antioxidants and Zinc in Patients with Age-related Macular Degeneration. Ophthalmology. 2013;120:2317-2323. ↑
- Chew EY, Klein ML, Clemons TE, et al. No Clinically Significant Association Between CFH and ARMS2 Genotypes and Response to Nutritional Supplements: AREDS Report No 38. Ophthalmology. 2014; 121(11):2173-2180. ↑
- Awh CC, Hawken S, Zanke BW. Treatment Response to Antioxidants and Zinc Based on CFH and ARMS2 Genetic Risk Allele Number in the Age-Related Eye Disease Study. Ophthalmology. 2015;122:162-169. ↑
- Chew EY, Klein ML, Clemons TE, et al. Genetic testing in persons with age-related macular degeneration and the use of the AREDS supplements: to test or not to test? Ophthalmology. 2015;122(1):212-215. ↑
- Stone EM, Aldave AJ, Drack AV, et al. Recommendations for Genetic Testing of Inherited Eye Diseases – 2014. Available at: https://www.aao.org/clinical-statement/recommendations-genetic-testing-of-inherited-eye-d. Accessed Sep 20, 2017. ↑
- Schwartz SG, Hampton BM, Kovach JL, Brantley MA. Genetics and age-related macular degeneration: a practical review for the clinician. Clin Ophthalmol. 2016;10:1229-1235. ↑
- Seddon JM, Silver RE, Rosner B. Response to AREDS supplements according to genetic factors: survival analysis approach using the eye as the unit of analysis. Br J Ophthalmol. 2016;100(12):1731-1737. ↑
- ArcticDx. ND. “AREDS Eye Supplements – Helpful or Harmful?” Available from: http://macularisk.com/amd-pharmacogenetics/areds-eye-supplements-helpful-or-harmful.html. Accessed on Sep 21, 2017. ↑
- Wong WL, Su X, Li X, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health 2014; 2: e106-16. ↑
- Klein R, Klein BEK, Linton KLP. Prevalence of Age-related Maculopathy. The Beaver Dam Eye Study. Ophthalmology. 1992;99:933-43. ↑
- Knobbe, Chris A. Ancestral Dietary Strategy to Prevent and Treat Macular Degeneration. Vervante, Springville, Utah, 2016, pp. 134-137. ↑
- Charlton KE, Russell J, Gorman E, et al. Fish, food security and health in Pacific Island countries and territories: a systematic literature review. BMC Public Health. 24 March, 2016. https://doi.org/10.1186/s12889-016-2953-9. ↑
- Food in Every Country. ND. “Islands of the Pacific.” Available at: http://www.foodbycountry.com/Germany-to-Japan/Islands-of-the-Pacific.html. Accessed Sep 26, 2017. ↑
- University of Hawai’i at Manoa Library. ND. “Traditional Pacific Island Crops: Coconut.” Available at: http://guides.library.manoa.hawaii.edu/paccrops/coconut. Accessed Sep. 25, 2017. ↑
- Hughes RG, Lawrence MA. Globalisation, food and health in Pacifid Island countries. Asia Pac J Clin Nutr. 2005;14(4):298-306. ↑
- Yasuda M, Kiyohara Y, Hata Y, et al. Nine-year incidence and risk factors for age-related macular degeneration in a defined Japanese population the Hisayama study. Ophthalmology. 2009;116(11):2135-40. ↑
- Nakata I, Yamashiro K, Nakanishi H, et al. Prevalence and characteristics of age-related macular degeneration in the Japanese population: the Nagahama study. Am J Ophthalmol. 2013;156(5):1002-1009. ↑
- Kanazawa M, Yoshike N, Osaka T, et al. Criteria and classification of obesity in Japan and Asia-Oceania. Asia Pac J Clin Nutr. 2002 Dec; 11 Suppl 8 S732-7. ↑
- Price, WA. Nutrition and Physical Degeneration: Eighth Edition. La Mesa, CA: Price-Pottenger Nutrition Foundation (2008), p. 294. ↑