Is Age-Related Macular Degeneration (AMD) Preventable – and Treatable – With Diet?
by Chris A. Knobbe, MD
Age-Related Macular Degeneration (AMD) and its associated vision loss is known to affect legendary actress Dame Judi Dench, 80, and famed novelist, Stephen King, 68. Both have spoken publicly of their eye conditions. Dench reports that she has trouble reading her lines for movies, while King reports no vision loss as yet. Dench and King are not outliers. They’re just a two of the many millions of people affected by this potentially devastating disease, which gradually steals the central vision.
AMD is the leading cause of irreversible vision loss in people over the age of 65, in developed nations.[1] By 1994, some 15 million Americans over the age of 50 were estimated to have been affected by AMD.[2] Globally, some 196 million people are expected to be afflicted with the disease by year 2020, with that number projected to rise to 288 million by 2040.[3] For people between 45 and 85 years of age, this translates to 8.69% with some degree of AMD.3 In 1992, in the United States, nearly one in three adults over the age of 75 was determined to be affected by AMD.[4]
Even worse, as of 2002 the World Health Organization (WHO) determined that 8.7% of the world’s blindness and severe vision loss, numbering some 14 million people, was secondary to AMD.[5]
The macula is the central retina, accounting for only four percent of the total retinal area. It is only 6 millimeters across – that is – almost exactly one-fourth of an inch. Arguably, this is the most important six millimeters in our bodies.
Orthodox ophthalmology has found many associations with AMD, but the underlying cause has remained elusive. As written in Albert & Jakobiec’s 1994 edition of Principles and Practice of Ophthalmology, which serves as a major reference for ophthalmologists, “Since the cause or causes of AMD are unknown, we lack the means for its prevention.” [6] This statement remains true for orthodox ophthalmology, today.
For decades, AMD has primarily been associated with aging (hence, the name, “age-related macular degeneration”) and, more recently, genetics. And although increased AMD prevalence has been associated with heart disease,[7] type 2 diabetes,[8] obesity,[9] and metabolic syndrome,[10] there generally has not been any suggestion that these conditions are the cause of AMD.
In August of 2016, at the Ancestral Health Symposium – 2016, for the first time publicly, I proffered the following hypothesis: The ‘displacing foods of modern commerce’ are the primary and proximate cause of AMD.
For those who are familiar with the late Weston A. Price, whom many nutrition researchers consider the ‘Father of Nutrition,’ the term ‘displacing foods of modern commerce’ will be quite familiar. This term equates essentially to refined white flour, refined sugars, most vegetable oils (primarily polyunsaturated oils), and trans fats – in short – man-made, processed foods.
I first developed this hypothesis in late 2013, but it would take nearly three years of investigative journalism, interviews, and our own fundamental research, all of which culminated in the authoring of a book on this subject. That book, Ancestral Dietary Strategy to Prevent and Treat Macular Degeneration, was published in September of 2016.
Why Diet – and Not Aging or Genetics – as the Cause of AMD?
In late 2013, it occurred to me that, if macular degeneration was all about aging and genetics, as orthodox ophthalmology asserts, then the prevalence of the disease should have been the same a century ago, as it is today – correct? This should be the case, since we generally believe that our DNA is stable over very long periods of time, i.e., up to many thousands of years. And our DNA, the master architectural plan of our bodies, is also generally believed to be nearly immutable. Evolutionary biologist and paleo diet founder, S. Boyd Eaton, MD, wrote “Our genetic makeup, especially that regarding our core metabolic and physiologic characteristics, has changed very little between the emergence of agriculture, roughly 10,000 years ago, and the present.” [11]
With that fundamental concept, I asked myself two questions: First, was AMD always as prevalent as it is today? And second, when could ophthalmologists even see the retina? The latter question, because obviously, ophthalmologists would have to visualize the retina in order to make the diagnosis, or even characterize, macular degeneration. If the evidence favored AMD as being an unusual or rare disorder in the past – and ophthalmologists were collectively able to visualize the macula simultaneously – then that evidence would strongly be in favor of an environmental factor at work. The suspected environmental factor, as we now know is the case with most chronic metabolic diseases such as heart disease, hypertension, type 2 diabetes, cancer, obesity, and numerous other diseases of civilization, is “Westernization” of the diet.[12]
The History of AMD in the U.S. — and Worldwide
It may come as a surprise to the lay public, but we physicians have virtually no education about the history of medicine, even within our own specialty. In fact, as far back 1896, just before the American Academy of Ophthalmology was founded, German physician Rudolph Virchow said, “It is one of the worst aspects of our present developmental stage of medicine that the historical knowledge of things diminishes with each generation of students. Even independent young researchers can normally be assumed to have a historical knowledge of no more than three to five years at a maximum. Anything published more than five years ago does not exist.” [13]
Virchow’s statement remains just as true today. In medical school, internship, and right through my three-year ophthalmology residency, I learned virtually nothing about the history of medicine, nor the history of ophthalmology. And, in fact, when I began to research the history of macular degeneration, I was stunned to find that I couldn’t find a single resource whereby the history of AMD, the single most common retinal condition of our time, had already been researched. That led me on a search that would take months to complete, digging up antiquated textbooks from the 1800’s as well as scientific papers published in the late 19th century and beyond. I did this with the assistance of reference librarians from around the world and many book stores, particularly those that held historical medical textbooks, which are few in number. It was a journey that was laborious, intensive, and long. But these relics from medical history held astonishing facts that would not only be germane to my hypothesis, but also turned out to support it.
So back to the question: When could ophthalmologists first visualize the retina? The answer: In 1851 – because of the genius of German born physician and physicist, Hermann von Helmholtz, who not only invented the ophthalmoscope, but published the design so that it could be reproduced by manufacturers.[14] The ophthalmoscope became the first device that eyecare providers would use to visualize the optic nerve, macula, vessels, and the rest of the retina. Within a decade, this technology had spread around the world. This also resulted in a number of retinal atlases having been produced during the 1850s and 1860s.[15]
Curiously, however, despite the fact that these atlas images virtually always included the macula, as it is in the center of the view through the ophthalmoscope, none of these images ever characterized anything resembling AMD. In fact, it would be 23 years following Helmholtz’ publication of the ophthalmoscope design before the first cases of macular degeneration were characterized. In 1874, London, England ophthalmologist, Jonathan Hutchinson described four cases that he had collected from his practice.[16] After another eleven years of silence on the subject, German ophthalmologist, Otto Haab, discussed the equivalent of macular degeneration in a lecture – in 1885.[17] Yet another decade later, Haab published a paper in which he had evaluated some 50,000 ophthalmic patient medical records and, from these, he determined that macular degeneration was as rare as myopic maculopathy and traumatic maculopathy. These two conditions are very rarely detected in the retina.[18] [19] For perspective, in 24 years of ophthalmology practice, I have witnessed less than a handful of these latter two conditions combined, yet I would typically see that many patients with AMD in any half-day of practice.
The literature remained almost silent on the condition of macular degeneration until about 1930, despite the fact that the optic nerve and retinal conditions were the subject of great discovery, numerous papers, and the attention of many book chapters. And in case one is left to wonder about widespread use of the ophthalmoscope, ophthalmologists Landolt and Snellen had collected some 86 versions of the ophthalmoscope by 1880, 140 versions by 1901 (on the 50th anniversary of Helmholtz design), and 200 models by 1913.[20]
In 1927, London, England ophthalmologist, Sir Stewart Duke-Elder, published his first comprehensive textbook of ophthalmology. The eminent Duke-Elder, who would become the most dominant force in ophthalmology for more than four decades, was not only revered, but prolific. His 1927 textbook was 340 pages in length, yet failed to even mention macular degeneration, though that was typical for textbooks of that era.[21] Thirteen years later, however, in Duke-Elder’s next comprehensive textbook of ophthalmology, he dedicated some 13 pages to the condition of macular degeneration, including 17 images, six of which were in full-color. He referred to macular degeneration as “a common cause of failure in central vision in old people.” [22] Obviously, by the 1930s, macular degeneration had risen from the status of medical rarity to a somewhat more common condition of the macula. Duke-Elder, however, did not mention any known or suspected degree of prevalence.
Though this is in part supposition, I believe it is fair to say that Duke-Elder was likely not even aware of the condition of age-related macular degeneration, or its equivalent, in the year 1927, however, the condition had become intimately familiar to him by the late 1930s.
By 1975, the first ever large-scale, epidemiologic study of the prevalence of AMD was completed, and this was the Framingham Eye Study.[23] In this particular study, in order to meet diagnostic criteria for AMD, subjects had to have vision loss to 20/30 or worse and to have drusen. Drusen are the yellow-white metabolic deposits that we see in the macula of those with AMD, and which are so characteristic of the disease. In the Framingham study, 8.8% of those subjects between 52 and 85 years of age were determined to have AMD, with 27.9% of those between 75 and 85 meeting the definition of disease.
This historical review and recent research indicate that AMD was a medical rarity between 1851 and 1930, and subsequently rose to epidemic proportions in the U.S. by 1975. Perhaps even more concerning, most developed nations have followed suit, developing high degrees of both incidence and prevalence of AMD in more recent decades. The question is: Why?
The ‘Displacing Foods of Modern Commerce’ – Historical View
Until 1880, it was nearly impossible to consume a nutrient-deficient diet, assuming one had enough food and a variety of food. History is very clear that all of the chronic metabolic diseases, i.e., “Westernized” diseases, such as heart disease, cancer, type 2 diabetes, and obesity, all of which are so prevalent today, were medical rarities at the turn of the 20th century.[24] Without question, there have always been some people whose nutrition has been poor, sometimes despite a near abundance of nutritious, natural food being available. This was likely the result of being poor, making poor food choices, war or confinement, drought, or perhaps, even conditions associated with poor food choices, such as alcoholism.
In 1880, however, for the first time, refined white wheat flour was produced on a large-scale, because that was the year that roller mill technology replaced stone mill technology for grinding wheat into flour. Roller mill technology could entirely remove the bran and the germ of the grain, thereby leaving behind only the endosperm. This type of flour, which was deemed highly desirable at the time, is referred to as “refined” because the roller-mill extraction may also remove the associated B vitamins, E vitamins, omega-3 and omega-6 fats, fiber, and minerals that are naturally found in wheat.[25] This was, chronologically, our second major refined, nutrient-deficient food, with refined sugar having been the first. Today, wheat accounts for 20% of the world’s diet.[26] By 2005, Loren Cordain, S. Boyd Eaton and colleagues found that 85.3% of the cereal grains consumed in the U.S., particularly including wheat, are now “highly processed refined grains.” [27]
Introduced just after the American Civil War in the U.S., in 1866, were the seed oils – generally referred to today as “vegetable oils.” The first of these was cottonseed oil.[28] This was soon followed by the hydrogenation and partial hydrogenation of cottonseed oil, producing the first ever artificially created trans-fat. The latter was introduced by Proctor & Gamble in 1911 under the name “Crisco,” which was marketed as “the healthier alternative to lard… and more economical than butter.”[29] This first commercially produced trans-fat, i.e., Crisco, remains on the market today.
The so-called “vegetable oils,” along with Crisco, would gradually supplant animal fats, such as butter, lard, and beef tallow. In fact, this was the manufacturers intent, i.e., to undersell the more expensive animal fats that had traditionally been used in cooking.
Loren Cordain and colleagues showed that, in the year 1900, the consumption of olive oil, essentially the only edible oil available at that time for most people, would have been in the range of 0.5 pounds per person per year.27 By 2005, however, the average American was consuming 86 pounds of added fats and oils per year, nearly 86% of which was vegetable oils and related products (shortening, margarine, cooking oils, etc.).[30] The remaining 14% came from butter, lard, and edible tallow. That is, in the year 1900, 99 percent of the added fats in cooking would have come from animal fats such as butter, lard, and beef tallow, whereas by 2005, that number had dropped to a mere 14 percent.
Sugar, our fourth and final major nutrient-deficient, processed food ingredient, had ever-increasing consumption from the 17th century until 1999, after which consumption decreased slightly. Following his historical research of sugar consumption, obesity researcher Stephan Guyenet, PhD, wrote “Wrap your brain around this: in 1822, we ate the amount of added sugar in one 12 ounce can of soda every five days, while today we eat that much sugar every seven hours.”[31] He found that we consumed 6.2 pounds of sugar per person per year in 1822, which rose to a high of 107.7 pounds per person per year, by 1999. This is 17-fold increase in the consumption of sugar during that period of time.31 In 1999, this amounted to an average consumption of 32 teaspoons per person per day.[32]
By 2009, 63 percent of U.S. food consumption was made up of processed, nutrient-deficient, potentially toxic foods, that is, consisting of refined grains (mostly refined wheat flour), vegetable oils, trans-fats, and sugar.[33] This is a recipe for metabolic disaster – the same recipe that has led to an epidemic of heart disease, cancer, metabolic syndrome, type 2 diabetes, hypertension, and in my opinion, AMD.
Synthetic Vitamins – Will They Rescue Patients From AMD?
More often than not, synthetic vitamins, i.e., those that come in pills, potions, bottles, and “fortified” foods, fail to deliver beneficial outcomes or their intended results. The fundamental scientific literature is riddled with failures in this regard, as evidenced by recent lectures on this subject by Howard Sesso, ScD, MPH, at the Harvard School of Public Health,[34] and Jeffrey Tice, MD, at the University of California San Francisco, Department of Medicine.[35]
But would synthetic vitamins, which I differentiate from those found in whole foods, be any different in preventing or treating AMD? With regard to the prevention of AMD, the Cochrane Collaboration evaluated four randomized controlled trials that included some 62,520 people. The results? In their words, “People who took these supplements were not at decreased (or increased) risk of developing AMD.” Their final conclusion: “There is accumulating evidence that taking vitamin E or beta-carotene supplements will not prevent or delay the onset of AMD. There is no evidence with respect to other antioxidant supplements, such as vitamin C, lutein, zeaxanthin, or any of the commonly marketed multivitamin combinations.” [36]
Next question: Do synthetic vitamin/multivitamin supplements help delay progression of AMD that is already established? Utilizing the fair and unbiased results of the Cochrane Collaboration once again, Cochrane found that there were 13 randomized controlled trials that attempted to answer this question. Of those thirteen, twelve showed no benefit. The Cochrane study reported, “The review of trials found that supplementation with antioxidants and zinc may be of modest benefit in people with AMD. This was mainly seen in one large trial {AREDS} that followed up participants for an average of six years. The other smaller trials with shorter follow-up do not provide evidence of any benefit. Although generally regarded as safe, vitamin supplements may have harmful effects.” [37]
The one trial where synthetic vitamins showed a benefit, the Age-Related Eye Disease Study (AREDS, or “AREDS 1 Trial”), published in 2001, evaluated some 3640 subjects, 55 to 80 years of age, who consumed either a combination of vitamins E and C, beta-carotene, zinc, and copper, or a placebo. For those in AMD categories 3 or 4, which is moderately advanced AMD in both eyes or advanced AMD in one eye, respectively, the results are reported as follows: “The risk reduction for those taking antioxidants plus zinc was 25%.”[38]
But, the approximate ‘25% reduction in AMD progression’ is a relative number, not absolute. What we want to know is what is our absolute risk reduction, because that is what is meaningful if we have AMD. So, let’s examine this further.
For those with category 3 or 4 macular disease, at 5 years from the onset of the study, the probability of progression to advanced AMD was 28% for those given placebo, 23% for those given antioxidants (vitamins E, C, and beta-carotene), 22% for those given zinc, and 20% for those given antioxidants and zinc (the AREDS formula).
From this, the difference between 20% and 28%, is just 8%. Eight percent is the absolute difference in numbers of patients progressing from intermediate AMD in both eyes or advanced AMD in one eye, to advanced AMD, during the five year follow-up. Eight percent of patients translates to 1 in 12.5, but since you cannot have half a person, this is actually one in 13.
That is, one in 13 was better, as a result of the AREDS formula.
And from this we get the Number Needed to Treat (NNT), which is also 13. That is, you will need to treat 13 patients with the AREDS formula for five years, for one patient to benefit. In the pharmacist’s National PBM Drug Monograph for Ocuvite Preservision, the NNT is reported as 12, but we’re splitting hairs here. They round down, since 1 in 12 sounds better than one in 13. Nevertheless, this is still a statement, that 12 subjects would have to be treated with the AREDS formula over a period of 5 years, for one to benefit, and this was the best case scenario. That is, 8% of subjects benefitted from taking AREDS supplement for 5 years.
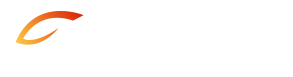
In patients with AMD categories 2, 3, or 4, which is much closer to considering all of those with AMD, the NNT was 20 for those taking the AREDS formula versus placebo. In this scenario, 20 subjects would need to take the AREDS formula for 5 years, for one to benefit. In this case, only 5% of subjects benefitted by taking AREDS formula for 5 years. Here is the table from the National PBM Drug Monograph:
Click here for the source file for the above data compilation table to download the PDF.
The AREDS 2 trial sought to determine whether the addition of the carotenoids, lutein and zeaxanthin, or the long chain omega-3 fatty acids, EPA and DHA, or both might further reduce the progression of AMD. In the authors’ own words, “Addition of lutein + zeaxanthin, DHA + EPA, or both to the AREDS formulation in primary analyses did not further reduce risk of progression to advanced AMD.” [39]
So the AREDS formula supplement appeared to benefit, in people with moderate AMD in both eyes or advanced AMD in one eye, one out of 12 subjects who took the supplements for 5 years, at least according to this one trial.
Recall that the other 12 trials, all of which were shorter in duration, found no benefit to the supplements. So we ophthalmologists generally recommended the “AREDS vitamins.”
But then ophthalmologist, Carl Awh, MD, and colleagues, assessed the AREDS results based on genetic profiles. They determined that those people with certain genetic profiles (high CFH and low ARMS2), which was 13% of the studied population, had a 135% higher chance of progressing to advanced stages of AMD – if they took the AREDS supplements.[40] [41] This is a more than doubling of the rate of progression – apparently caused by taking the supplements. Now what?
AMD Prevalence Versus a Westernized Diet – Original Research
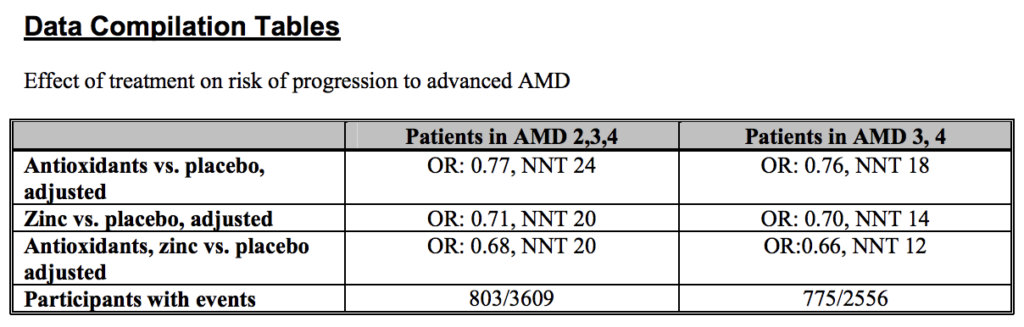
To evaluate the effect of Westernization of the diet, versus the development and prevalence of AMD, my colleague, Marija Stojanoska, MSc and I, mined the two greatest proxy markers of processed food, sugar and vegetable oils – from the Food and Agricultural Organization of the United Nations (FAO) databases. We then plotted that data against AMD prevalence, in 25 nations. Click here to reference all of the graphs and data below, in our published paper.
In this article, three representative graphs for three nations will be presented. Note that we’ve separated vegetable oils into “Harmless Vegetable Oils,” which is the saturated oils (coconut, palm, and palm kernel oils, plus olive oil and flaxseed oil) and the “Harmful Oils,” which are the oils containing the most polyunsaturated oils (soybean, corn, canola, cottonseed, sunflower, safflower, rapeseed, grapeseed, and rice bran oils). Those oils deemed to be of intermediate risk, due to the presence of both polyunsaturated and monounsaturated components, included peanut, sesame, and high oleic sunflower and high oleic safflower oils, were categorized among the “harmful oils,” however, their proportions are relatively very small in most Western cultures, and there is significant evidence that peanut and sesame oils are far safer, having been consumed by Asian cultures with an apparent high degree of tolerance for many decades.
Below is the correlative data for sugar and vegetable oils, versus AMD prevalence, in the U.S.:
Note that total vegetable oil consumption was around two grams a day from 1900 until about 1909, and then jumped up to 10 g/person/day and climbed from that point forward, eventually reaching 80 g/person/day by 2010. Sugar consumption was already at about 80 grams per day by 1900, climbing to a high of nearly 200 g/day by 1999. As you will recall, AMD prevalence was negligible from 1851 until the 1930s and as one can see from the graph, was at epidemic proportions by the 1970s and beyond.
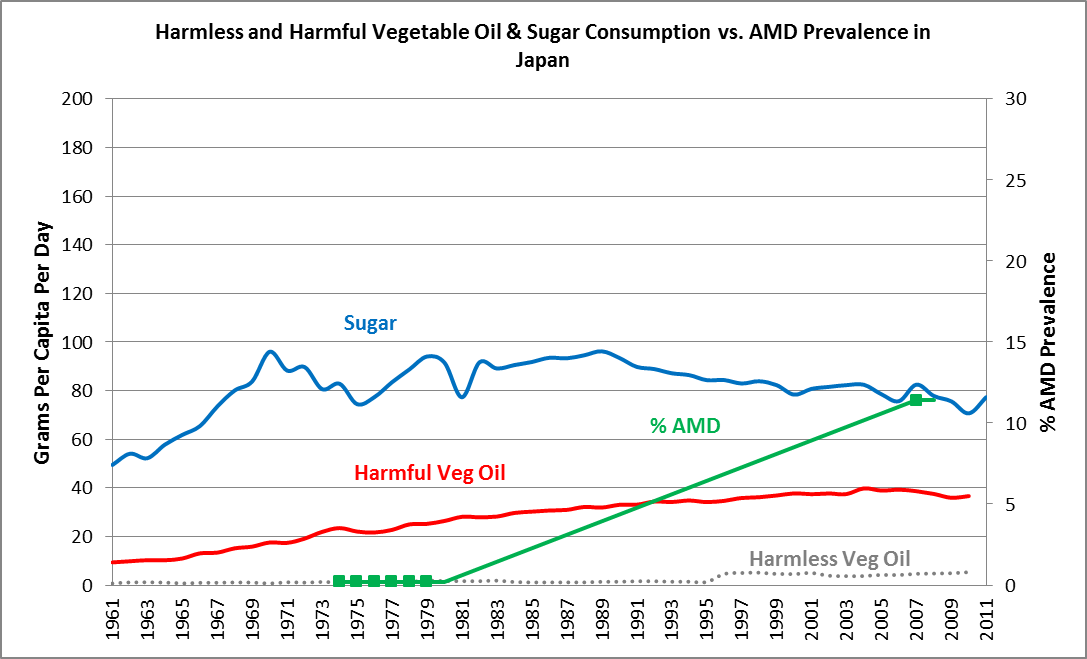
Japan is perhaps one of the greatest examples where we see Westernization of the diet in just the past five decades and, within a period of just under 30 years, we see the rise of AMD from the status of extreme medical rarity – to epidemic proportions. Note that the “Harmful Vegetable Oils” elevated from 1961 forward, rising 4.5-fold between 1961 and 2005. Sugar consumption rose from approximately 50 grams per day in 1961, to over 90 grams a day by the late 1960s, and remained nearly at that level through 2011. Westernization of Japan’s diet was associated with an increase in AMD prevalence from 0.2% between 1974 and 1979, to 11.4% by 2007, an increase of 57-fold in the prevalence of AMD, in a period of no more than 30 years!
Ask yourself, “How could a 57-fold increase in AMD prevalence, in a period of 30 years, be explained by aging and genetics?”
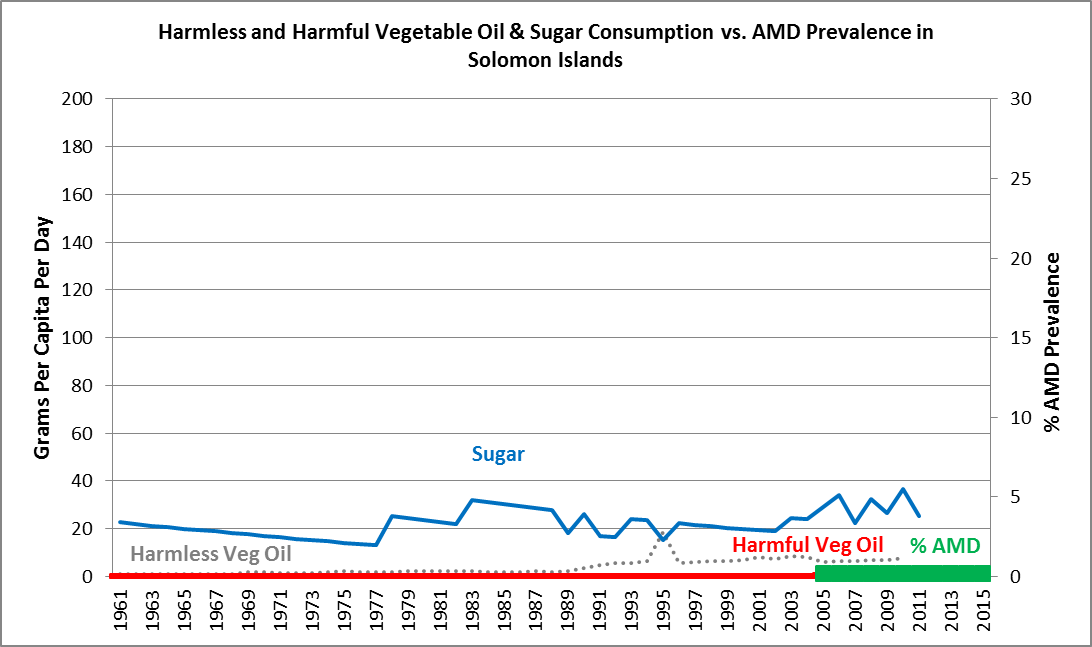
In the Solomon Islands, we see that sugar consumption, from 1961 forward, remains extremely low at around 20 grams per day, while harmful vegetable oil consumption remains at almost negligible levels from 1961 forward. And the prevalence of AMD is approximately 0.2% — that is, almost non-existent, for the past ten years. The situation is almost identical in Samoa, while sugar consumption is much higher in Kiribati, but AMD prevalence remains a medical rarity.
Conclusions and Dietary Recommendations
We’ve seen that, historically, macular degeneration was an extreme medical rarity from 1851 until the 1930s. During that era, three of our four major nutrient-deficient processed food elements were introduced – refined white flour, in 1880, polyunsaturated vegetable oils, just after the American Civil War ending in 1865, and trans-fats, in 1911. Sugar consumption, our fourth nutrient-deficient, processed food, was on the rise. By the 1930s, macular degeneration was on the radar of ophthalmologists as a significant entity. By the 1970s, AMD was at epidemic proportions in the U.S. and U.K., with many nations subsequently following suit.
Every shred of evidence that I can find – supports the hypothesis that it is the ‘displacing foods of modern commerce’ that are the primary and proximate cause of AMD.
The prevention of this disease – as well as the treatment – is to remove those elements from the diet that truly make it “Westernized,”, i.e., refined (added sugars), refined white flours, vegetable oils, and trans fats, and consume only elements of our traditions, i.e., our own native, traditional diets, whatever one chooses for that to be. This means eliminating man-made, processed, nutrient-deficient, and toxic food components.
This would mean, generally, that one should consume a diet rich in 100% pasture-raised meats (beef, lamb, chicken), wild-caught fish, pastured eggs, possibly fruit and vegetables (if well tolerated, and organic if possible), possibly very small amounts of nuts and seeds, and critically, some “sacred” foods of our ancestors, such as beef or chicken liver, fish eggs (roe), and/or extra virgin cod liver oil (EVCLO) and very likely, pastured, grass-fed butter, and/or raw, grass-fed whole milk. These so-called “sacred foods” are rich in the fat-soluble vitamins, A, D, and K2, which are not well-distributed in the food supply, but which are incredibly and vitally important to preventing degenerative disease. Please note, age-related macular degeneration, as its name implies, is a degenerative disease.
My preference and recommendation is to choose the wild or pastured versions of animal meats and eggs, whenever possible, and organic versions of grains, fruits, and vegetables, if affordable. However, even the concentrated animal feeding operation (CAFO) raised versions of these animals and non-organically raised fruits and vegetables, will be markedly superior for health, as compared to man-made, processed, nutrient-deficient foods, such as most fast-foods and prepared and packaged foods.
As for the AREDS formula vitamins, I advise against them, in favor of an ancestral diet.
Finally, in my humble opinion, macular degeneration should no longer be called ‘age-related macular degeneration’ (AMD), but rather, Diet-Related Macular Degeneration (DMD), as we have recommended in our hypothesis introducing paper, published in the November issue of the highly regarded journal, Medical Hypotheses.
Chris A. Knobbe, MD, is ophthalmologist and Associate Clinical Professor Emeritus, University of Texas Southwestern Medical Center, in Dallas, Texas, as well as the Founder and President of Cure AMD Foundation™. Dr. Knobbe is author of the book, Ancestral Dietary Strategy to Prevent & Treat Macular Degeneration, which is available at this link. Dr. Knobbe may be reached directly via the contact form at CureAMD.org.
References
- Van Bol L, Rasquin F. [Age-related macular degeneration]. Rev Med Brux 2014; 35(4): 265-70. ↑
- Egan KM, Seddon JM. Age-Related Macular Degeneration: Epidemiology. In: Albert & Jakobiec, Principles and Practice of Ophthalmology. Philadelphia, PA: W.B. Saunders Company; 1994: 1266. ↑
- Wong WL, Su X, Li X, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health 2014; 2: e106-16. ↑
- Klein R, Klein BE, Linton KL. Prevalence of age-related maculopathy. The Beaver Dam Eye Study. Ophthalmology. 1992; 99: 933-43. ↑
- Resnikoff S, Pascolini D, Etya’ale D, et al. Global data on visual impairment in the year 2002. Bulletin of the World Health Organization 2004; 82: 844-851. ↑
- Egan KM, Seddon JM. (1994) Albert & Jakobiec: Principles and Practice of Ophthalmology. Basic Sciences (Philadelphia: W.B. Saunders Co.), p. 1273. ↑
- Sun C, Klein R, Wong TY. Age-related macular degeneration and risk of coronary heart disease and stroke: the Cardiovascular Health Study. Ophthalmology. 2009; 116(10): 1913-1919. ↑
- Klein R, Deng Y, Klein BE, et al. Cardiovascular disease, its risk factors and treatment, and age-related macular degeneration: Women’s health initiative sight exam ancillary study. Am J Ophthalmol. 2007; 143(3): 473-483. ↑
- Cheung N, Wong TY. Obesity and eye diseases. Surv Ophthalmol. 2007; 52(2): 180-95. ↑
- Maralani HG, Tai BC, Wong TY, et al. Metabolic syndrome and risk of age-related macular degeneration. Retina. 2015; 35(3): 459-66. ↑
- Muehlenbein, Michael P. (Editor) Human Evolutionary Biology. Cambridge, New York, Cambridge University Press, 2010, p. 491. ↑
- Cordain, Loren. The Paleo Answer. Hoboken, New Jersey: John Wiley and Sons, Inc., 2012. ↑
- Albert, Daniel M. The History of Ophthalmology. Cambridge, Massachusetts, Blackwell Science, Inc., 1996. p. xvi (Preface). ↑
- Albert, Daniel M. The History of Ophthalmology. Blackwell Science, Inc., Cambridge, Massachusetts, 1996, p. 76. ↑
- Albert, Daniel M., Edwards, Diane D. The History of Ophthalmology. Cambridge, Massachusetts, Blackwell Science, 1996. Pp. 191, 195-196. ↑
- Hutchinson J, Tay W. Symmetrical central choroido-retinal disease occurring in senile persons. R Lond Ophthalmic Hosp Rep J Ophthalmic Surg. 1874; 8: 231-244. ↑
- Haab, O. Zentralblatt für prakrische Augenheilkunde v. 9, p. 383-4, 1885. ↑
- Haab O. Atlas und Grundriss der Ophthalmoskopie und ophthalmoskopischen Diagnostik. Atlas and outline of ophthalmoscopy and ophthalmoscopic diagnosis. München, Lehmann; 1895. ↑
- Haab O. Ueber die Erkrankung der Macula lutea. On the disease of the macula lutea. Siebenter Periodischer Internationaler Ophthalmologen-Congress Heidelberg. 1888, p. 429. ↑
- Keeler CR. A Brief History of the Ophthalmoscope. The Royal College of Ophthalmologists, London, UK, Accepted for publication 16 June 2003. Available at: Optometry in Practice 2003; Vol 4: p. 138. ↑
- Duke-Elder, W. Stewart. Recent Advances in Ophthalmology. Philadelphia, P. Blakiston’s Son & Co., 1927. ↑
- Duke-Elder, WS. Textbook of Ophthalmology – Duke-Elder, Vol. III, Diseases of the Inner Eye. St. Louis: The C.V. Mosby Company, 1940. p. 2372 – 2373. ↑
- Kahn HA, Leibowitz HM. Ganley JP, et al. The Framingham Eye Study I. Outline and major prevalence findings. Am J Epidemiol. 1977; 106(1): 17-32. ↑
- Knobbe, Chris. Ancestral Dietary Strategy to Prevent & Treat Macular Degeneration. Springville, Utah: Vervante Corporation, 2016, pp.98-103. ↑
- Slavin JL, Jacobs D, Marquart L. Grain Processing and Nutrition. Critical Reviews in Biotechnology. 2001; 21(1): 49-66. ↑
- Brenchley R, Spannagl M, Pfeifer M, et al. Analysis of the bread wheat genome using whole genome shotgun sequencing. Nature 2012; 491: 705-710. ↑
- Cordain L, Eaton SB, et al. Origins and evolution of the Western diet: health implications for the 21st century. Am J Clin Nutr. 2005; 81: 341-54. ↑
- Nixon, H.C. The Rise of the American Cottonseed Oil Industry. Journal of Political Economy. 1930; 38(1): 73-85 ↑
- Proctor & Gamble – A Company History – 1837 – Today. Available online: https://www.pg.com/translations/history_pdf/english_history.pdf ↑
- Dietary Assessment of Major Trends in U.S. Food Consumption, 1970 – 2005. USDA Economic Research Service. Bulletin Number 33, March 2008. ↑
- Guyenet, Stephan. “By 2606, the US Diet will be 100 Percent Sugar.” Whole Health Source, Nutrition and Health Science. Feb 18, 2012. Available at: www.wholehealthsource.org. ↑
- “Profiling Food Consumption in America.” USDA Economic Research Service, Factbook, Chapter 2. ND. Available at: http://www.usda.gov/factbook/chapter2.pdf ↑
- U.S. Food Consumption As A Percent Of Calories – 2009. USDA Economic Research Service, 2009; Available at: http://www.ers.usda.gov. ↑
- Sesso, Howard. “Food and Vitamins and Supplements! Oh My! – Longwood Seminar.” Harvard Medical School. Published Mar 8, 2013. Available at: https://www.youtube.com/watch?v=j9E8bUIEsIo ↑
- Tice, Jeffrey. “Vitamins and Supplements: An Evidence-Based Approach.” Published Oct 29, 2013. Available at: http://www.uctv.tv. ↑
- Evans JR, Lawrenson JG. Antioxidant vitamin and mineral supplements for preventing age-related macular degeneration (Review). The Cochrane Collaboration. The Cochrane Library, 2012, Issue 6. ↑
- Evans JR, Lawrenson JG. Antioxidant vitamins and mineral supplements to slow the progression of age-related macular degeneration. Cochrane. 14 Nov. 2012. ↑
- Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol. 2001; 119(10): 1417-36. ↑
- Age-Related Eye Disease Study 2 Research Group. Lutein + zeaxanthin and omega-3 fatty acids for age-related macular degeneration: the Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA. 2013; 309(19): 2005-15. ↑
- Awh CC, Lane AM, Hawken S, et al. CFH and ARMS2 genetic polymorphisms predict response to antioxidants and zinc in patients with age-related macular degeneration. Ophthalmol. 2013; 120(11): 2317-23. ↑
- Harrison, Laird. “Supplements to Slow Macular Degeneration May Backfire.” Medscape. August 13, 2014. ↑